Abstract
Rationale
Patients with obsessive compulsive disorder (OCD) demonstrate impaired cognition in some selected domains. Although serotoninergic dysfunction has been implicated in OCD, recent evidence suggests that dopamine may play a role as well.
Objective
The aim of the study was to evaluate learning and working memory in OCD and to determine the effects of dopaminergic manipulations on these capacities.
Methods
Visuospatial associative memory and spatial and verbal working memory were examined in 18 nondepressed patients with OCD and 18 matched healthy controls. The study further investigated whether acute administration of dopamine D2/D3 receptor agonist and antagonist would differentially modulate cognition in OCD. Each participant underwent the cognitive battery three times in a randomized double-blind, placebo-controlled crossover design.
Results
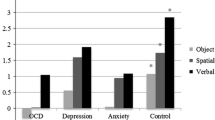
Significant impairments in patients compared with controls were noted on the Cambridge Neuropsychological Test Automated Battery (CANTAB) paired associates learning (PAL) and a measure of sustained attention (rapid visual information processing, RVIP) that persisted across all sessions, with deficient strategy in the CANTAB spatial working memory task in the first session alone. Although the dopamine D2/D3 agonist, pramipexole, led to poorer performance on the PAL and RVIP tasks, no differential effects were noted between the two groups. No significant effects were noted for the D2/D3 antagonist, amisulpride.
Conclusions
The results are consistent with a specific associative memory deficit in OCD that remained robust despite possible practice effects and compensatory strategies and point to abnormal medial temporal lobe involvement in OCD in addition to the previously implicated frontostriatal loops, with no clear evidence of D2 receptor mediation.

Similar content being viewed by others
References
Abbas AI, Hedlund PB, Huang XP, Tran TB, Meltzer HY, Roth BL (2009) Amisulpride is a potent 5-HT7 antagonist: relevance for antidepressant actions in vivo. Psychopharmacology (Berl) 205:119–128
APA (2000) Diagnostic and statistical manual of mental disorders (DSM-IV-TR), 4 revisedth edn. American Psychiatric Association, Arlington
Aronowitz BR, Hollander E, DeCaria C, Cohen L, Saoud JB, Liebowitz MR, Rosen WG (1994) Neuropsychology of obsessive compulsive disorder: preliminary findings. Neuropsychiatry Neuropsychol Behav Neurol 7:81–86
Barrett SL, Bell R, Watson D, King DJ (2004) Effects of amisulpride, risperidone and chlorpromazine on auditory and visual latent inhibition, prepulse inhibition, executive function and eye movements in healthy volunteers. J Psychopharmacol 18:156–172
Beck AT, Steer RA, Ball R, Ranieri WF (1996) Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess 67:588–597
Berthier ML, Kulisevsky J, Gironell A, Heras JA (1996) Obsessive–compulsive disorder associated with brain lesions: clinical phenomenology, cognitive function, and anatomic correlates. Neurology 47:353–361
Blackwell AD, Sahakian BJ, Vesey R, Semple JM, Robbins TW, Hodges JR (2003) Detecting dementia: novel neuropsychological markers of preclinical Alzheimer’s disease. Dement Geriatr Cogn Disord 17:42–48
Bloch MH, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB, Leckman JF (2006) A systematic review: antipsychotic augmentation with treatment refractory obsessive–compulsive disorder. Mol Psychiatry 11:622–632
Boone KB, Ananth J, Philpott L, Kaur A, Djenderedjian A (1991) Neuropsychological characteristics of nondepressed adults with obsessive–compulsive disorder. Neuropsychiatry Neuropsychol Behav Neurol 4:96–109
Burns GL, Keortge SG, Formea GM, Sternberger LG (1996) Revision of the Padua Inventory of obsessive compulsive disorder symptoms: distinctions between worry, obsessions, and compulsions. Behav Res Ther 34:163–173
Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ (2005) The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev 29:399–419
Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2007) A neuropsychological comparison of obsessive–compulsive disorder and trichotillomania. Neuropsychologia 45:654–662
Christensen KJ, Kim SW, Dysken MW, Hoover KM (1992) Neuropsychological performance in obsessive–compulsive disorder. Biol Psychiatry 31:4–18
Cohen LJ, Hollander E, DeCaria CM, Stein DJ, Simeon D, Liebowitz MR, Aronowitz BR (1996) Specificity of neuropsychological impairment in obsessive–compulsive disorder: a comparison with social phobic and normal control subjects. J Neuropsychiatry Clin Neurosci 8:82–85
Dahabra S, Ashton CH, Bahrainian M, Britton PG, Ferrier IN, McAllister VA, Marsh VR, Moore PB (1998) Structural and functional abnormalities in elderly patients clinically recovered from early- and late-onset depression. Biol Psychiatry 44:34–46
De Jager C, Blackwell AD, Budge MM, Sahakian BJ (2005) Predicting cognitive decline in healthy older adults. Am J Geriatr Psychiatry 13:735–740
Deckersbach T, Savage CR, Dougherty DD, Bohne A, Loh R, Nierenberg A, Sachs G, Rauch SL (2005) Spontaneous and directed application of verbal learning strategies in bipolar disorder and obsessive–compulsive disorder. Bipolar Disord 7:166–175
Delis DC, Levin BE, Kramer JH (1987) Verbal-learning and memory deficits in Parkinson Disease. J Clin Exp Neuropsychol 9:17
Denys D, de Geus F, van Megen HJ, Westenberg HG (2004a) A double-blind, randomized, placebo-controlled trial of quetiapine addition in patients with obsessive–compulsive disorder refractory to serotonin reuptake inhibitors. J Clin Psychiatry 65:1040–1048
Denys D, van der Wee N, Janssen J, De Geus F, Westenberg HGM (2004b) Low level of dopaminergic D-2 receptor binding in obsessive–compulsive disorder. Biol Psychiatry 55:1041–1045
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS (1989) The Yale-Brown obsessive compulsive scale. I. Development, use, and reliability. Arch Gen Psychiatry 46:1006–1011
Goodman WK, Price LH, Delgado PL, Palumbo J, Krystal JH, Nagy LM, Rasmussen SA, Heninger GR, Charney DS (1990) Specificity of serotonin reuptake inhibitors in the treatment of obsessive–compulsive disorder—comparison of fluvoxamine and desipramine. Arch Gen Psychiatry 47:577–585
Gould RL, Arroyo B, Brown RG, Owen AM, Bullmore ET, Howard RJ (2006) Brain mechanisms of successful compensation during learning in Alzheimer disease. Neurology 67:1011–1017
Graybiel AM, Rauch SL (2000) Toward a neurobiology of obsessive–compulsive disorder. Neuron 28:343–347
Hamidovic A, Kang UJ, de Wit H (2008) Effects of low to moderate acute doses of pramipexole on impulsivity and cognition in healthy volunteers. J Clin Psychopharmacol 28:45–51
Hedlund PB (2009) The 5-HT7 receptor and disorders of the nervous system: an overview. Psychopharmacology (Berl) 206:345–354
Henseler I, Gruber O, Kraft S, Krick C, Reith W, Falkai P (2008) Compensatory hyperactivations as markers of latent working memory dysfunctions in patients with obsessive–compulsive disorder: an fMRI study. J Psychiatry Neurosci 33:209–215
Hesse S, Muller U, Lincke T, Barthel H, Villmann T, Angermeyer MC, Sabri O, Stengler-Wenzke K (2005) Serotonin and dopamine transporter imaging in patients with obsessive–compulsive disorder. Psychiatry Res Neuroimaging 140:63–72
Hollander E, Liebowitz MR, Rosen WG (1991) Neuropsychiatric and neuropsychological studies in obsessive–compulsive disorder. In: Zohar J, Insel T, Rasmussen S (eds) Psychobiology of obsessive-compulsive disorder. Springer, New York, pp 126–145
Kapur S, Remington G (1996) Serotonin–dopamine interaction and its relevance to schizophrenia. Am J Psychiatry 153:466–476
Korff S, Harvey BH (2006) Animal models of obsessive–compulsive disorder: rationale to understanding psychobiology and pharmacology. Psychiatr Clin North Am 29:371–390
Kuelz AK, Hohagen F, Voderholzer U (2004) Neuropsychological performance in obsessive–compulsive disorder: a critical review. Biol Psychiatry 65:185–236
Legangneux E, McEwen J, Wesnes KA, Bergougnan L, Miget N, Canal M, L’Heritier C, Pinquier JL, Rosenzweig P (2000) The acute effects of amisulpride (50 mg and 200 mg) and haloperidol (2 mg) on cognitive function in healthy elderly volunteers. J Psychopharmacol 14:164–171
Leplow B, Murphy R, Nutzinger DO (2002) Specificity of conditional associative-learning deficits in obsessive–compulsive disorder (OCD) and non-OCD anxiety disorders. J Clin Exp Neuropsychol 24:792–805
Luciana M, Collins PF (1997) Dopaminergic modulation of working memory for spatial but not object cues in normal humans. J Cognitive Neurosci 9:330–347
Luciana M, Collins PF, Depue RA (1998) Opposing roles for dopamine and serotonin in the modulation of human spatial working memory functions. Cereb Cortex 8:218–226
Mehta MA, Sahakian BJ, McKenna PJ, Robbins TW (1999) Systemic sulpiride in young adult volunteers simulates the profile of cognitive deficits in Parkinson's disease. Psychopharmacology (Berl) 146:162–174
Mehta MA, Swainson R, Ogilvie AD, Sahakian J, Robbins TW (2001) Improved short-term spatial memory but impaired reversal learning following the dopamine D(2) agonist bromocriptine in human volunteers. Psychopharmacology (Berl) 159:10–20
McDougle CJ, Epperson CN, Pelton GH, Wasylink S, Price LH (2000) A double-blind, placebo-controlled study of risperidone addition in serotonin reuptake inhibitor-refractory obsessive–compulsive disorder. Arch Gen Psychiatry 57:794–801
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET (2008) Integrating evidence from neuroimaging and neuropsychological studies of obsessive–compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev 32:525–549
Metin O, Yazici K, Tot S, Yazici AE (2003) Amisulpride augmentation in treatment resistant obsessive–compulsive disorder: an open trial. Hum Psychopharmacol 18:463–467
Michopoulos I, Zervas IM, Pantelis C, Tsaltas E, Papakosta VM, Boufidou F, Nikolaou C, Papageorgiou C, Soldatos CR, Lykouras L (2008) Neuropsychological and hypothalamic-pituitary-axis function in female patients with melancholic and non-melancholic depression. Eur Arch Psychiatry Clin Neurosci 258:217–225
Milliery M, Bouvard M, Aupetit J, Cottraux J (2000) Sustained attention in patients with obsessive–compulsive disorder: a controlled study. Psychiatry Res 96:199–209
Moritz S, Kloss M, Jahn H, Schick M, Hand I (2003) Impact of comorbid depressive symptoms on nonverbal memory and visuospatial performance in obsessive–compulsive disorder. Cogn Neuropsychiatry 8:261–272
Muller J, Roberts JE (2005) Memory and attention in obsessive–compulsive disorder: a review. J Anxiety Disord 19:1–28
Murphy R, Nutzinger DO, Paul T, Leplow B (2004) Conditional-associative learning in eating disorders: a comparison with OCD. J Clin Exp Neuropsychol 26:190–199
Nelson HE (1982) The national adult reading test manual. NFER-Nelson, Windsor
Nielen MMA, Den Boer JA (2003) Neuropsychological performance of OCD patients before and after treatment with fluoxetine: evidence for persistent cognitive deficits. Psychol Med 33:917–925
Nielen MM, den Boer JA, Smid HG (2009) Patients with obsessive–compulsive disorder are impaired in associative learning based on external feedback. Psychol Med 39:1519–1526
Nordahl TE, Benkelfat C, Semple WE, Gross M, King AC, Cohen RM (1989) Cerebral glucose metabolic rates in obsessive compulsive disorder. Neuropsychopharmacology 2:23–28
Olley A, Malhi G, Sachdev P (2007) Memory and executive functioning in obsessive–compulsive disorder: a selective review. J Affect Disord 104:15–23
Osterrieth PA (1944) Le test de copie d’une figure complex. Arch Psychol 30:206–356
Owen AM, Downes JJ, Sahakian BJ, Polkey CE, Robbins TW (1990) Planning and spatial working memory following frontal lobe lesions in man. Neuropsychologia 28:1021–1034
Owen AM, Sahakian BJ, Semple J, Polkey CE, Robbins TW (1995) Visuospatial short-term recognition memory and learning after temporal-lobe excisions, frontal-lobe excisions or amygdalo-hippocampectomy in man. Neuropsychologia 33:1–24
Park SB, Coull JT, McShane RH, Young AH, Sahakian BJ, Robbins TW, Cowen PJ (1994) Tryptophan depletion in normal volunteers produces selective impairments in learning and memory. Neuropharmacology 33:575–588
Perani D, Garibotto V, Gorini A, Moresco RM, Henin M, Panzacchi A, Matarrese M, Carpinelli A, Bellodi L, Fazio F (2008) In vivo PET study of 5HT(2A) serotonin and D(2) dopamine dysfunction in drug-naive obsessive–compulsive disorder. Neuroimage 42:306–314
Peretti CS, Danion JM, Kauffmann-Muller F, Grange D, Patat A, Rosenzweig P (1997) Effects of haloperidol and amisulpride on motor and cognitive skill learning in healthy volunteers. Psychopharmacology (Berl) 131:329–338
Pessiglione M, Seymour B, Flandin G, Dolan RJ, Frith CD (2006) Dopamine-dependent prediction errors underpin reward-seeking behavior in humans. Nature 442:1042–1045
Pizzagalli DA, Evins AE, Schetter EC, Frank MJ, Pajtas PE, Santesso DL, Culhane M (2008) Single dose of a dopamine agonist impairs reinforcement learning in humans: behavioral evidence from a laboratory-based measure of reward responsiveness. Psychopharmacology 196:221–232
Porter RJ, Gallagher P, Thompson JM, Young AH (2003) Neurocognitive impairment in drug-free patients with major depressive disorder. Br J Psychiatry 182:214–220
Purcell R, Maruff P, Kyrios M, Pantelis C (1998) Neuropsychological deficits in obsessive–compulsive disorder: a comparison with unipolar depression, panic disorder, and normal controls. Arch Gen Psychiatry 55:415–423
Rauch SL, Wedig MM, Wright CI, Martis B, McMullin KG, Shin LM, Cannistraro PA, Wilhelm S (2007) Functional magnetic resonance imaging study of regional brain activation during implicit sequence learning in obsessive–compulsive disorder. Biol Psychiatry 61:330–336
Rektorová I, Rektor I, Bares M, Dostál V, Ehler E, Fanfrdlová Z, Fiedler J, Klajblová H, Kulist’ák P, Ressner P, Svátová J, Urbánek K, Velísková J (2005) Cognitive performance in people with Parkinson’s disease and mild or moderate depression: effects of dopamine agonists in an add-on to l-dopa therapy. Eur J Neurol 12:9–15
Robins TW (2010) From behavior to cognition: functions of the mesostriatal, mesolimbic and mesocortical dopamine systems. In: Iversen LL, Ivesen SD, Dunnett SB, Bjorklund A (eds) Dopamine handbook. Oxford University Press, New York, pp 203–214
Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA (1984) Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 41:949–958
Rosenzweig P, Canal M, Patat A, Bergougnan L, Zieleniuk I, Bianchetti G (2002) A review of the pharmacokinetics, tolerability and pharmacodynamics of amisulpride in healthy volunteers. Hum Psychopharmacol 17:1–13
Sahakian BJ, Morris RG, Evenden JL, Heald A, Levy R, Philpot M, Robbins TW (1988) A comparative study of visuospatial memory and learning in Alzheimer-type dementia and Parkinson’s disease. Brain 111(Pt 3):695–718
Samuels ER, Hou RH, Langley RW, Szabadi E, Bradshaw CM (2006a) Comparison of pramipexole and amisulpride on alertness, autonomic and endocrine functions in healthy volunteers. Psychopharmacology 187:498–510
Samuels ER, Hou RH, Langley RW, Szabadi E, Bradshaw CM (2006b) Comparison of pramipexole and modafinil on arousal, autonomic, and endocrine functions in healthy volunteers. J Psychopharmacol 20:756–770
Savage CR, Keuthen NJ, Jenike MA, Brown HD, Baer L, Kendrick AD, Miguel EC, Rauch SL, Albert MS (1996) Recall and recognition memory in obsessive–compulsive disorder. J Neuropsychiatry Clin Neurosci 8:99–103
Savage CR, Deckersbach T, Wilhelm S, Rauch SL, Baer L, Reid T, Jenike MA (2000) Strategic processing and episodic memory impairment in obsessive compulsive disorder. Neuropsychology 14:141–151
Saxena S, Rauch SL (2000) Functional neuroimaging and the neuroanatomy of obsessive–compulsive disorder. Psychiatr Clin North Am 23:563–586
Schmidtke K, Schorb A, Winkelmann G, Hohagen F (1998) Cognitive frontal lobe dysfunction in obsessive–compulsive disorder. Biol Psychiatry 43:666–673
van den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, van Balkom AJ, van Hartskamp J, Barkhof F, van Dyck R (2005) Frontal-striatal dysfunction during planning in obsessive–compulsive disorder. Arch Gen Psychiatry 62:301–309
van der Wee NJA, Ramsey NF, Jansma JM, Denys DA, van Megen H, Westenberg HMG, Kahn RS (2003) Spatial working memory deficits in obsessive compulsive disorder are associated with excessive engagement of the medial frontal cortex. Neuroimage 20:2271–2280
van der Wee NJA, Ramsey NF, van Megen H, Denys D, Westenberg HGM, Kahn RS (2007) Spatial working memory in obsessive–compulsive disorder improves with clinical response: a functional MRI study. Eur Neuropsychopharmacol 17:16–23
Von Huben SN, Davis SA, Lay CC, Katner SN, Crean RD, Taffe MA (2006) Differential contributions of dopaminergic D1- and D2-like receptors to cognitive function in rhesus monkeys. Psychopharmacology (Berl) 188:586–596
Wechsler D (1981) Wechsler adult intelligence scale, revised. Psychological Corporation, San Antonio
Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, Newman SC, Oakley-Browne MA, Rubio-Stipec M, Wickramaratne PJ et al (1994) The cross national epidemiology of obsessive compulsive disorder. The Cross National Collaborative Group. J Clin Psychiatry 55(Suppl):5–10
Westenberg HGM, Fineberg NA, Denys D (2007) Neurobiology of obsessive–compulsive disorder: serotonin and beyond. CNS Spectr 12:14–27
Wright CE, Sisson TL, Ichhpurani AK, Peters GR (1997) Steady-state pharmacokinetic properties of pramipexole in healthy volunteers. J Clin Pharmacol 37:520–525
Zielinski CM, Taylor MA, Juzwin KR (1991) Neuropsychological deficits in obsessive–compulsive disorder. Neuropsychiatry Neuropsychol Behav Neurol 4:110–126
Acknowledgments
The authors wish to thank the participants who took part in the study. The study was funded by a research grant to TWR from GlaxoSmithKline. The Behavioral and Clinical Neuroscience Institute is cofunded by a grant from the MRC and the Wellcome Trust. SM-Z is funded by a Wellcome Trust Program Grant to TWR. KJC is employed by and is a shareholder in P1vital Ltd., whose clients include several pharmaceutical companies. KDE is supported by a Betty Behrens Clare Hall Research Fellowship. UM has consulted for Janssen-Cilag; has received research support from Alexander von Humboldt Foundation, Janssen-Cilag, Medical Research Council (MRC), and Isaac Newton Trust; and has received honoraria and support to attend and/or lecture at scientific meetings from Bristol-Meyers Squibb, Eli-Lilly, Janssen-Cilag, Lundbeck, Shire, and UCB Pharma. NAF has consulted for Lundbeck, GlaxoSmithKline, Servier, and Bristol Myers Squibb; has received research support from Lundbeck, GlaxoSmithKline, Astra Zeneca, Wellcome, ECNP, and Cephalon; has received honoraria and support to attend and/or lecture at scientific meetings from Janssen, Jazz, Lundbeck, Servier, Astra Zeneca, Cephalon, and Wyeth. EB is employed half-time by the University of Cambridge and half-time by the GlaxoSmithKline and owns shares in GSK. BJS consults for Cambridge Cognition Ltd. and a number of pharmaceutical companies and owns shares in CeNeS. TWR consults for Cambridge Cognition, Pfizer, Lilly, Lundbeck, Allon Therapeutics, and GlaxoSmithKline and currently holds grant funding from GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sharon Morein-Zamir and Kevin J. Craig have joint authorship.
Rights and permissions
About this article
Cite this article
Morein-Zamir, S., Craig, K.J., Ersche, K.D. et al. Impaired visuospatial associative memory and attention in obsessive compulsive disorder but no evidence for differential dopaminergic modulation. Psychopharmacology 212, 357–367 (2010). https://doi.org/10.1007/s00213-010-1963-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-010-1963-z