Abstract
Summary
We performed a cost-effectiveness analysis of four vitamin D supplementation strategies for primary prevention of hip fracture among the elderly population and found that the most cost-effective strategy was screening for vitamin D insufficiency followed by adequate treatment to attain a minimum 25(OH) serum level.
Introduction
Vitamin D supplementation has a demonstrated ability to reduce the incidence of hip fractures. The efficiency of lifetime supplementation has not yet been assessed in the population over 65 years without previous hip fracture. The objective was to analyze the efficiency of various vitamin D supplementation strategies for that population.
Methods
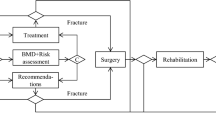
A Markov micro-simulation model was built with data extracted from published studies and from the French reimbursement schedule. Four vitamin D supplementation strategies were evaluated on our study population: (1) no treatment, (2) supplementation without any serum level check; (3) supplementation with a serum level check 3 months after initiation and subsequent treatment adaptation; (4) population screening for vitamin D insufficiency followed by treatment based on the vitamin D serum level.
Results
“Treat, then check” and “screen and treat” were two cost-effective strategies and dominated “treat without check” with incremental cost-effectiveness ratios of €5,219/quality-adjusted life-years (QALY) and €9,104/QALY, respectively. The acceptability curves showed that over €6,000/QALY, the “screen and treat” strategy had the greatest probability of being cost-effective, and the “no treatment” strategy would never be cost-effective if society were willing to spend over €8,000/QALY. The sensitivity analysis showed that among all parameters varying within realistic ranges, the cost of vitamin D treatment had the greatest effect and yet remained below the WHO cost-effectiveness thresholds.
Conclusions
Population screening for vitamin D insufficiency followed by treatment based on the vitamin D serum level is the most cost-effective strategy for preventing hip fracture occurrence in the population over 65 years old.



Similar content being viewed by others
References
Mithal A, Wahl DA, Bonjour JP et al (2009) Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 20:1807–1820. doi:10.1007/s00198-009-0954-6
Borgström F, Lekander I, Ivergård M et al (2013) The International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS)—quality of life during the first 4 months after fracture. Osteoporos Int 24:811–823. doi:10.1007/s00198-012-2240-2
Bleibler F, Konnopka A, Benzinger P et al (2013) The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany—a demographic simulation model. Osteoporos Int 24:835–847. doi:10.1007/s00198-012-2020-z
McGowan B, Casey MC, Silke C et al (2013) Hospitalisations for fracture and associated costs between 2000 and 2009 in Ireland: a trend analysis. Osteoporos Int 24:849–857. doi:10.1007/s00198-012-2032-8
(2011) La vitamine D chez l’adulte: recommandations du GRIO. La Presse Médicale 40:673–682. doi: 10.1016/j.lpm.2011.04.001
Bischoff-Ferrari HA, Willett WC, Orav EJ et al (2012) A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 367:40–49. doi:10.1056/NEJMoa1109617
Sattar N, Welsh P, Panarelli M, Forouhi NG (2012) Increasing requests for vitamin D measurement: costly, confusing, and without credibility. Lancet 379:95–96. doi:10.1016/S0140-6736(11)61816-3
Sonnenberg FA, Beck JR (1993) Markov models in medical decision making. Med Decis Mak 13:322–338. doi:10.1177/0272989X9301300409
Siebert U, Alagoz O, Bayoumi AM et al (2012) State-transition modeling: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force—3. Value Health 15:812–820. doi:10.1016/j.jval.2012.06.014
Development Core Team R (2011) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Kanis JA, Johnell O, Oden A et al (2004) The risk and burden of vertebral fractures in Sweden. Osteoporos Int 15:20–26. doi:10.1007/s00198-003-1463-7
Jönsson B, Christiansen C, Johnell O et al (1996) Cost-effectiveness of fracture prevention in established osteoporosis. Scand J Rheumatol Suppl 103:30–38, discussion 39–40
Burström K, Johannesson M, Diderichsen F (2001) Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 10:621–635
[INED] Table de mortalité. http://www.ined.fr/fr/pop_chiffres/france/mortalite_causes_deces/table_mortalite/. Accessed 4 April 2013
Haentjens P, Magaziner J, Colón-Emeric CS et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390. doi:10.1059/0003-4819-152-6-201003160-00008
Maravic M, Taupin P, Landais P, Roux C (2011) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int 22:797–801. doi:10.1007/s00198-010-1255-9
Ryg J, Rejnmark L, Overgaard S et al (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977–2001. J Bone Miner Res 24:1299–1307. doi:10.1359/jbmr.090207
Bischoff-Ferrari HA, Willett WC, Wong JB et al (2009) Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med 169:551–561. doi:10.1001/archinternmed.2008.600
UVEDOSE 100 000 UI SOL BUV. http://www.vidal.fr/Medicament/uvedose-17128.htm. Accessed 26 April 2013
ameli.fr - l’Assurance Maladie en ligne. http://www.ameli.fr/. Accessed 26 April 2013
Sabaté E (2003) Adherence to long-term therapies: evidence for action. World Health Organization
Doubilet P, Begg CB, Weinstein MC et al (1985) Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach. Med Decis Making 5:157–177
Pasta DJ, Taylor JL, Henning JM (1999) Probabilistic sensitivity analysis incorporating the bootstrap an example comparing treatments for the eradication of Helicobacter pylori. Med Decis Making 19:353–363. doi:10.1177/0272989X9901900314
JAMAevidence | Glossary: C. http://jamaevidence.com/glossary/C. Accessed 24 June 2013
Fenwick E (2005) A guide to cost-effectiveness acceptability curves. Br J Psychiatry 187:106–108. doi:10.1192/bjp.187.2.106
Eddy DM, Hollingworth W, Caro JJ et al (2012) Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-7. Value Health 15:843–850. doi:10.1016/j.jval.2012.04.012
WHO | Table: Threshold values for intervention cost-effectiveness by Region. In: WHO. http://www.who.int/choice/costs/CER_levels/en/index.html. Accessed 8 April 2013
Kanis JA, Johnell O, Oden A et al (2000) Risk of hip fracture derived from relative risks: an analysis applied to the population of Sweden. Osteoporos Int 11:120–127. doi:10.1007/PL00004173
Willis MS (2002) The health economics of calcium and vitamin D3 for the prevention of osteoporotic hip fractures in Sweden. Int J Technol Assess Health Care 18:791–807. doi:10.1017/S0266462302000600
Fleurence RL (2004) Cost-effectiveness of fracture prevention treatments in the elderly. Int J Technol Assess Health Care 20:184–191
Lee RH, Weber T, Colón-Emeric C (2013) Comparison of cost-effectiveness of vitamin D screening with that of universal supplementation in preventing falls in community-dwelling older adults. J Am Geriatr Soc. doi:10.1111/jgs.12213
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281. doi:10.1056/NEJMra070553
Souberbielle JC, Body J-J, Lappe JM et al (2010) Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: recommendations for clinical practice. Autoimmun Rev 9:709–715. doi:10.1016/j.autrev.2010.06.009
Autier P, Gandini S (2007) Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med 167:1730–1737. doi:10.1001/archinte.167.16.1730
Looker AC (2013) Serum 25-hydroxyvitamin D and risk of major osteoporotic fractures in older U.S. adults. J Bone Miner Res 28:997–1006. doi:10.1002/jbmr.1828
Kruk ME, Schwalbe N (2006) The relation between intermittent dosing and adherence: preliminary insights. Clin Ther 28:1989–1995. doi:10.1016/j.clinthera.2006.12.011
Rouillon V, Dubourg G, Gauvain JB et al (2012) Vitamin D insufficiency: evaluation of an oral standardized supplementation using 100,000 IU vials of cholecalciferol, depending on initial serum level of 25OH vitamin D. Joint Bone Spine 79:399–402. doi:10.1016/j.jbspin.2011.09.004
Bischoff-Ferrari HA, Shao A, Dawson-Hughes B et al (2010) Benefit–risk assessment of vitamin D supplementation. Osteoporos Int 21:1121–1132. doi:10.1007/s00198-009-1119-3
Sanders KM, Stuart AL, Williamson EJ et al (2010) Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 303:1815–1822. doi:10.1001/jama.2010.594
Farrell C, Soldo J, Williams P, Herrmann M (2012) 25-Hydroxyvitamin D testing: challenging the performance of current automated immunoassays. Clin Chem Lab Med 50:1953–1963. doi:10.1515/cclm-2012-0522
Barake M, Daher RT, Salti I et al (2012) 25-Hydroxyvitamin D assay variations and impact on clinical decision making. J Clin Endocrinol Metab 97:835–843. doi:10.1210/jc.2011-2584
Stepman HCM, Vanderroost A, Van Uytfanghe K, Thienpont LM (2011) Candidate reference measurement procedures for serum 25-hydroxyvitamin D3 and 25-hydroxyvitamin D2 by using isotope-dilution liquid chromatography–tandem mass spectrometry. Clin Chem 57:441–448. doi:10.1373/clinchem.2010.152553
Sempos CT, Vesper HW, Phinney KW et al (2012) Vitamin D status as an international issue: national surveys and the problem of standardization. Scand J Clin Lab Invest Suppl 243:32–40. doi:10.3109/00365513.2012.681935
Vernay M, Sponga M, Salavane B et al (2012) Vitamin D status in the French adult population: the French Nutrition and Health Survey (ENNS, 2006–2007). BEH - Bulletin d’Epidémiologie Hebdomadaire 189–197
ATIH: Agence Technique de l’Information sur l’Hospitalisation. http://www.atih.sante.fr/. Accessed 2 March 2013
(2011) Choix méthodologiques pour l’évaluation économique à la HAS
Heaney RP, Davies KM, Chen TC et al (2003) Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77:204–210
Acknowledgments
The authors are deeply indebted to Ms Karen Berg Brigham (URC Eco Ile-de-France (AP-HP), Paris, France) for her insightful comments on the manuscript.
Conflicts of interest
All authors received fees for this work by Merck Sharp Dohme Laboratories France, either as a consulting fee, fees for participation in review activities, or support for travel to meetings for the study. Kevin Zarca reports no relevant financial activities outside this study. Isabelle Durand-Zaleski reports the following as relevant financial activities outside this study: consultancy fees (BMS, Sanofi, Medtronic, Abbott), payment for lectures (BMS, Sanofi), payment for development of educational presentations (BMS, Abbott). Christian Roux reports the following as relevant financial activities outside this study: advisory board membership (MSD, Lilly, Novartis, AMGEN), grants (Lilly, Bongrain, MSD), payment for lectures (MSD, Lilly, AMGEN, UCB). Jean-Claude Souberbielle reports no relevant financial activities outside this study. Anne-Marie Schott reports no relevant financial activities outside this study.
Thierry Thomas reports the following as relevant financial activities outside this study: consultancy fees (AMGEN, Genévrier, GSK, Lilly, Merck, Novartis, Servier), payment for lectures (AMGEN, Genévrier, GSK, Lilly, Merck, Novartis, Servier), grants (Amgen, Chugaï, Merck, Novartis, Pfizer, Roche, Servier, UCB, and Warner-Chilcott). Patrice Fardellone reports the following as relevant financial activities outside this study: board membership (Amgen, MSD, Candia, Roche, Roche-Chugaï), grants (Roche-Chugaï), payment for lectures (Abbvie, Lilly, Pfizer, BMS, UBS, Servier, Ipsen). Claude-Laurent Benhamou reports the following as relevant financial activities outside this study: board membership (Novartis, Lilly, Roche), consultancy (Rottapharm), grants (AMGEN, Servier).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 134 kb)
Rights and permissions
About this article
Cite this article
Zarca, K., Durand-Zaleski, I., Roux, C. et al. Cost-effectiveness analysis of hip fracture prevention with vitamin D supplementation: a Markov micro-simulation model applied to the French population over 65 years old without previous hip fracture. Osteoporos Int 25, 1797–1806 (2014). https://doi.org/10.1007/s00198-014-2698-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2698-1