Abstract
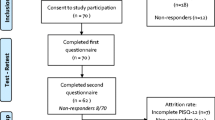
The aim of this study was to develop the short form of a condition-specific, reliable, validated and self-administered instrument to evaluate sexual function in women with pelvic organ prolapse and/or urinary incontinence. The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire –12 (PISQ-12) was developed from the data of 99 of 182 women surveyed to create the long form (PISQ-31). An additional 46 patients were recruited for further validation. All subsets regression analysis identified 12 items likely to predict PISQ-31 scores. Short form scores underwent correlation analysis with long form, Incontinence Impact Questionnaire – 7 (IIQ-7), Sexual History Form –12 (SHF-12) and Symptom Questionnaire (SQ) scores. Test–retest reliability was checked with a subset of 20 patients. All subsets regression analysis with R>0.92 identified 12 items that predicted PISQ-31 scores. Short form scores were highly correlated with long form scores (R=0.75–0.95). Correlations of the PISQ-12 with SHF-12 (R=–0.66 and –0.68) and IIQ-7 (R=–0.38 and –0.54) scores were similar to correlation of the PISQ-31 with these other measures. Reliability was moderate to high, with weighted κ values from 0.56 to 0.93. PISQ-12 scores were lower in patients with low sexual function as measured on the SHF-12 (P <0.001), and lower in women with depression as measured on the SQ (P <0.001). The PISQ-12 is a validated and reliable short form that evaluates sexual function in women with urinary incontinence and/or pelvic organ prolapse and predicts PISQ-31 scores. It is able to distinguish women with poor sexual function as measured on the SHF-12.
Similar content being viewed by others
References
Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C (2001) A new instrument to measure sexual function in women with urinary incontinence and/or pelvic organ prolapse. Am J Obstet Gynecol 184:552–558
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA, and the Continence Program for Women Research Group (1995) Short forms to assess life quality and symptoms distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodyn 14:131–139
Creti L, Fichten CS, Brender W (1998) Functioning. In: Davis CM, Yaber WH, Bauserman R, Schreer G, Davis SL (eds) Handbook of sexuality-related measures, 2nd edn. Sage, Thousand Oaks, pp 261–267
Kellner R, Sheffield BF (1973) A self-rating scale of distress. Psych Med 3:88–100
Weber AM, Walters MD, Schover LR, Mitchinson A (1995) Sexual function in women with uterovaginal prolapse and urinary incontinence. Obstet Gynecol 85:483–487
SAS Institute Inc.(1999) SASSTAT User’s Guide, Version 8. : SAS Institute, Cary, NC, 1310
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. John Wiley and Sons, New York, p 218
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Comment: For decades, clinicians and researchers have described treatment ‘success’ in our field as resolution of either anatomic defects or of urinary of fecal leakage. We have all had patients with perfect anatomic support after a prolapse operation who were unhappy because of problems with pain, leakage, defecation or sexual function. Yet, considering these and other quality of life issues as part of the definition of treatment success is a recent development. The emphasis on the importance of assessing various quality of life indicators is snow-balling, yet our efforts to do so have been hampered by the absence of good, easy to administrate, reliable and valid tools. The short form of the PISQ is an eagerly awaited tool that fills this void. From a research prospective, information derived from responses to this questionnaire will allow us to understand the effect of various treatments on sexual function, arguably one of the most important and least investigated domains of quality of life. When completed by patients in a clinical setting, the PISQ-12 provides a template for clinicians to discuss sexuality with patients, and to suggest appropriate interventions. In developing the long and short forms of this instrument, the authors have set a high standard for others developing quality of life instruments to strive for.
Study supported by NCRR-GCRC Grant # M01 RR00997
Presented at American Urogynecologic Society annual meeting in Hilton Head, South Carolina, USA, 2000
An erratum to this article can be found at http://dx.doi.org/10.1007/s00192-004-1167-3
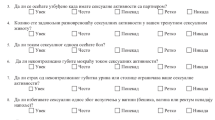
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Rogers, R.G., Coates, K.W., Kammerer-Doak, D. et al. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J 14, 164–168 (2003). https://doi.org/10.1007/s00192-003-1063-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-003-1063-2