Abstract
Purpose
To study the epidemiology and return to play characteristics of anterior and posterior ankle impingement syndromes (AAIS and PAIS) over 18 consecutive seasons in male professional soccer players.
Methods
Between the 2001–2002 and 2018–2019 seasons, 120 European soccer teams were followed prospectively for various seasons. Time loss injuries and player exposures were recorded individually in 6754 unique players. Injury incidence and burden were reported as the number of injuries and days absence per 1000 h with 95% confidence intervals (CIs). Injury severity was reported as median absence in days with the interquartile range (IQR).
Results
Out of 25,462 reported injuries, 93 (0.4%) were diagnosed as AAIS (38%) or PAIS (62%) in 77 players. AAIS and PAIS were similar regarding injury characteristics except for a greater proportion of AAIS having a gradual onset (69% vs.47%; P = 0.03) and being re-injuries (31% vs. 9%; P = 0.01). Impingement syndromes resulted in an overall incidence of 0.03 injuries (95% CI 0.02–0.03) per 1000 h and an injury burden of 0.4 absence days per 1000 h. PAIS incidence was significantly higher than that for AAIS [0.02 (95% CI 0.002–0.03) vs. 0.01 (95% CI 0.005–0.01) injuries per 1000 h (RR = 1.7). The absence was significantly longer in AAIS than in PAIS [10 (22) vs. 6 (11) days; P = 0.023]. Impingement syndromes that presented with a gradual onset had longer absences in comparison to impingement with an acute onset [8 (22) vs. 5 (11) days; P = 0.014]. Match play was associated with a higher incidence and greater injury burden than training: 0.08 vs. 0.02 injuries per 1000 h (RR 4.7), respectively, and 0.9 vs. 0.3 days absence per 1000 h (RR 2.5).
Conclusion
Ankle injuries are frequent in men’s professional soccer and ankle impingement is increasingly recognized as a common source of pain, limited range of motion, and potential time loss. In our study, ankle impingement was the cause of time loss in less than 0.5% of all injuries. PAIS was more frequently reported than AAIS, but AAIS was associated with more absence days and a higher re-injury rate than PAIS. The findings in this study can assist the physician in best practice management on ankle impingment syndromes in professional football.
Level of evidence
II.
Similar content being viewed by others
Introduction
The annual socioeconomic loss of soccer injuries’ costs are over $US 30 billion worldwide [29] with the ankle region as the fifth most commonly injured location, representing 13% of all injuries in soccer [27]. Player contact is a predominant cause of foot and ankle injuries (32–74%), but injuries also occur without player contact [6, 9, 18, 27, 28]. Ankle impingement is recognized as a common source of pain, limited range of motion, and potential time loss in soccer [6, 16, 22].
Ankle impingement is considered a syndrome and can be due to a broad range of pathologies and etiologies. They may present as acute traumatic injuries, but more commonly as gradual-onset conditions due to repetitive stress [11, 22, 28, 30]. While ankle impingement syndromes can be classified in detail according to the anatomical zone into anterior, anterolateral, anteromedial, posterolateral, and posteromedial, most practitioners categorize them, for simplicity, into either anterior ankle impingement syndrome (AAIS) or posterior ankle impingement syndrome (PAIS) [11]. AAIS was first recognized by Morris, who named it “athlete’s ankle” in 1943, and later described as the “footballer’s ankle” by McMurray in 1950 [15, 16, 18]. It is more commonly a bony impingement of tibiotalar osteophytes [21] that has been reported to affect up to 60% of professional soccer players [14]. PAIS, on the other hand, arises more commonly due to forced or repetitive plantarflexion of the ankle [25], which stresses the posterior ankle structures in the tibiocalcaneal interval narrowed by bony structures such as os trigonum, which is present in 7–25% of the general population [3, 8, 20].
The objective of this study was to investigate the epidemiology and return to play characteristics of AAIS and PAIS over 18 consecutive seasons in male professional soccer players.
Materials and methods
Written informed consents were collected from all participating players in accordance with the Declaration of Helsinki. The general study protocol was reviewed and approved by the UEFA Football Development Division and the UEFA Medical Committee. Individual ethical approval was also obtained from the ethical National review authorities in Denmark, Norway and Sweden (#01-062, #M240-09, and #S-06188).
This is a substudy of a long-term prospective cohort study evaluating men's professional soccer in Europe since 2001, the Union of European Football Associations (UEFA) Elite Club Injury Study (ECIS) [24]. The present study includes data from 18 consecutive seasons of male professional soccer between 2001 and 2019. During the study period, a total of 6754 players from 120 teams representing 25 countries were included. Most of the presented data were collected as part of the ECIS, but since ankle impingement is relatively infrequent, data from five other similar cohorts were also included (the English Premier League, European Artificial Turf Teams, the Swedish First League, the Danish First League, and the Nordic Football Injury Audits) as has been described previously [1].
Exposure and injury registration
Data collection was undertaken in accordance with the 2006 consensus statement on how to conduct injury surveillance research in soccer [22] and in line with the recent 2020 International Olympic Committee (IOC) consensus statement [2]. The overall study methodology has previously been described in detail [7].
In brief, all first team players in the included teams were invited to participate in the study. At the beginning of every season, teams appointed a contact person within their medical team to be responsible for collecting data and communicating with the study group. Player baseline data were collected at inclusion on an annual basis. All individual player exposures during supervised training sessions and matches were recorded on standard attendance records. Time loss injuries were registered on standard injury cards containing information about the type, location and circumstances of the injury. The appointed contact person reported attendance records and injury cards monthly to the study group that checked the reports and sent feedback to the teams to clarify any missing or unclear data. No specific diagnostic criteria for AAIS and PAIS were used, and it was up to the medical staffs to classify the injuries and refer for imaging or any other consultations needed. All injuries were given a diagnostic code by the study group per the Orchard Sports Injury Classification System (OSICS) 10 [19]. Injury was defined as any physical complaint sustained by a player that resulted from a soccer match or soccer training and led to the player being unable to take a full part in future soccer training or match play. Other relevant injury definitions for this substudy are highlighted in Table 1.
Statistical analysis
Data were analyzed using SPSS (IBM SPSS Statistics for Windows, V.26.0, IBM Corp, Armonk, New York, USA). Player demographics are reported with descriptive statistics using mean ± standard deviation (SD) and proportions. Injury incidence was calculated as the number of injuries per 1000 h of exposure ((Σ injuries/Σ exposure hours) × 1000) with corresponding 95% confidence interval (CI). Injury burden was calculated as the number of absence days per 1000 h of exposure ((Σ days absence/Σ exposure hours) × 1000). Rate ratio (RR) was calculated with 95% CI and tested for significance with Z-statistics. Injury severity was defined as the number of days of absence and presented as median with interquartile range (IQR). The Mann–Whitney U test was used to compare days of absence for different injury categories. The χ2 test was used to compare the proportions of categorical variables, while Students t test was used to compare the mean age, height, and weight between players suffering AAIS and PAIS. The significance level was set at P < 0.05.
Results
During the 18-season period, a total of 3,686,838 h of exposure and 25,462 injuries were reported. 93 AAIS and PAIS syndromes (0.4%) were recorded in 77 players. Eleven players sustained two to four syndrome presentations each during the study period. The right ankle was affected in 50 cases (54%) and the left ankle in 41 cases (44%), while only 2 cases were bilateral (2%). The mean age at the time of the presentation was 25.4 ± 4.2 years. There were no significant differences in baseline characteristics between players who suffered AAIS and PAIS (Table 2).
Injury characteristics
AAIS and PAIS represented 35 (38%) and 58 (62%) of the ankle impingement cases, with the majority having a gradual onset (both n = 51, 55%) and occurred during training (Table 3). Sixteen (18%) cases were considered as exacerbation of symptoms. AAIS and PAIS were similar with regard to injury characteristics with the exception of a greater proportion of AAIS being re-injuries [11 (32%) vs. 5 (9%); P < 0.01] and having a gradual onset [24 (69%) vs. 27 (47%); P = 0.03]. Information about player contact was collected from the 2004/05 season onward and was available for 76 of 93 injuries. Out of those 76 impingement injuries, there was a noncontact injury mechanism in 53 (69%) of the injuries with no difference in the mechanisms between AAIS and PAIS (Table 3).
Return to play and injury severity
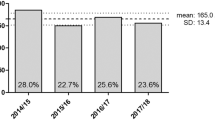
The median absence following an ankle impingement injury was 7 (IQR 16) days and 15 (16%) of the injuries were severe with > 28 days on the sidelines (Fig. 1 and Table 4).
The median absence was significantly longer in AAIS than PAIS [10 (22) vs. 6 (11) days; P = 0.023]. Gradual-onset injuries had significantly longer median absence compared with acute-onset injuries [8 (22) vs. 5 (11) days; P = 0.014].
Injury incidence and injury burden
The overall incidence of ankle impingement was 0.03 injuries (95% CI 0.02–0.03) per 1000 h. The incidence during match play was fivefold higher than during training [0.08 (95% CI 0.06–0.10) injuries per 1000 match hours vs. 0.02 injuries (95% CI 0.01–0.02) per 1000 training hours, RR 4.7 (95% CI 3.1–7.1)].
The incidence of PAIS was almost twofold higher than AAIS [0.02 (95% CI 0.001–0.02) injuries per 1000 h vs. 0.01 (95% CI 0.01–0.01) injuries per 1000 h, RR 1.7 (95% CI 1.1–2.5)]. This difference was mainly seen during match play [0.05 (95% CI 0.04–0.08) vs. 0.02 (95% CI 0.01–0.04) injuries per 1000 match hours, RR 2.5 (95% CI 1.3–4.9)]. No difference was seen during training [0.01 (95% CI 0.01–0.01) vs. 0.01 (95% CI 0.00–0.01) injuries per 1000 training hours, RR 1.2 (95% CI 0.7–2.1)]. A total of 1517 days of absence were reported due to ankle impingement (1046 days due to training injuries and 471 days due to match injuries). This represents an overall injury burden of 0.4 days per 1000 h, with 0.2 days per 1000 h calculated for both AAIS and PAIS (Table 5).
Discussion
The principal findings of this study were that PAIS occurred more frequently than AAIS and presented relatively more frequently with a gradual onset, whereas AAIS led to longer average absence and more re-injuries.
We calculated from Tables 4 and 5 that the total nr of absence days for AAIS was 770 and for PAIS 696. The number of days the players are absent is the key message that the coaches are listening to and the fact that PAIS has almost the same consequences for a team as the more well-known AAIS, might be a new and useful information.
Return to play
The present study found that soccer players with ankle impingement were able to return to play (RTP) at a median of 7 days (10 days in AAIS and 6 days in PAIS, respectively) following the injury occurrence, with only 16% of the injuries requiring longer than 28 days to recover. Importantly, our data included both injuries with nonsurgical and surgical treatment, whereas a few other studies have reported RTP details on surgically treated PAIS in soccer players exclusively. For example, Lopez-Valerio et al. [12] reported on 20 professional soccer players in Brazil who were treated arthroscopically for PAIS, and reported a mean RTP to the previous level of activity at an average of 46.9 days. Similarly, Calder et al. [4] reported an average of 34 days to return to training and 41 days to RTP in elite soccer players following arthroscopic surgery of PAIS. They also reported a sooner return in players with soft tissue rather than bony impingements. Finally, Kudaş et al. [10] reported an average RTP at 36 days of nonsurgical treatment in elite Turkish soccer players with PAIS. Murawski and Kennedy [17] reported RTP at a mean of 7 weeks (5–13 weeks) post-arthroscopic debridement of AAIS in a mixed population. The days of absence in the current study are fewer than reported in the literature and are to be interpreted with caution due to the lack of treatment data and detailed pathology (e.g., soft tissue vs bony impingement).
In the present study, AAIS led to significantly greater days of absence than PAIS. While such a comparison was not the main objective of this study, it could potentially be explained by the treatment strategy. In a previous study, AAIS had a higher probability of failure of nonsurgical management and thus requiring surgery, in comparison to 60% chance of success in PAIS after nonsurgical treatment [20]. Another possible cause for our findings is that soft tissue impingement, which is more common in PAIS, results in quicker recovery than bony causes of impingement. In the aforementioned series of 27 professional soccer players who underwent PAIS arthroscopic treatment, Calder et al. [4] reported a quicker return to training in soft tissue impingement in comparison to bony impingement (28 days vs. 40 days, respectively). Moreover, arthroscopic management of PAIS is considered to be safer in terms of nerve injuries than anterior arthroscopy needed for AAIS [12, 20, 23, 26].
Injury incidence
The overall incidence of symptomatic ankle impingement was 0.03 cases per 1000 h, with PAIS being 1.7 times more common than AAIS. Interestingly, the incidence was almost five times higher during match play compared with training. This could be attributed to the more unpredictable and aggressive style of play during matches, and similar findings were described by Lubberts et al. [13] who found that syndesmotic ankle injuries in professional soccer players were 13 times more frequent during match play compared with training.
Re-injury was identified as a repeated period of time loss due to AAIS or PAIS within the same season as a previous identical injury. In this paper, the re-injury variable was based on what was reported by teams. Teams were instructed to report injuries as re-injuries when a player suffered a second period of absence due to an injury of the same type and affecting the same location as a previous index injury.
Etiology of impingement syndromes
Multiple theories have been proposed regarding the etiology of AAIS, and a significant contribution to our understanding of the pathology has been done by Tol and van Dijk [24] in the 1990s and early 2000s. The earlier theory, first described by McMurray in 1950, attributed it to the traction forces on the anterior ankle capsule during forced plantar flexion, leading to the formation of anterior tibiotalar osteophytes and subsequent soft tissue proliferation and impingement [15, 25]. However, this theory has its limitations and has been disputed in favor of repetitive dorsiflexion and microtrauma [10, 15, 29]. An anatomical study by Tol and van Dijk [25] found the attachment of the anterior capsule to be on average 4 mm proximal to the cartilage. Likewise, a few other studies found the capsule to also be around 6 mm proximal to the site of the tibial spur, and arthroscopic examination has shown the spurs to be within the ankle joint and not in the joint capsule. Our results that the majority of ankle impingements had a gradual onset and AAIS was more common than PAIS support the subsequent theory of direct repetitive microtrauma and the findings of the biomechanical study by Tol et al. [25], where they concluded that the impact of a soccer ball to the anteromedial side of the cartilaginous rim generated sufficient forces to cause damage [5, 30].
Prevention and early recognition of impingement syndromes
Walls et al. highlighted the importance of injury and re-injury prevention and early recognition of ankle injuries in soccer players to optimize outcomes and reduce absence from sport [29]. Proper warmup, stretching, sufficient recovery, proprioception, and neuromuscular exercises are paramount for injury prevention. Additionally optimizing field conditions can further reduce injury incidence, especially non-contact injuries. Artificial turf, longer cleats, and dry hardened turf can increase the shoe–surface friction and thus increase the risk of ankle injuries [29]. An 18% recurrence rate and total a of 1517 days of absence due to ankle impingement were shown by our results, which represent an injury burden of 0.4 days absence per 1000 h. Hence, more organized efforts to prevent ankle impingement syndromes are required.
The clinical relevance of the findings in this study is that the provided epidemiological data on AAIS and PAIS in elite soccer can guide the clinician toward the best evidence-based ankle impingment management.
Unfortunately, this study presents several limitations. First, the injury form did not record the diagnostic tests and examination findings of all players and was not able to record data of all potentially important variables. The diagnosis was made by the medical teams of each soccer team and is consequently subject to biases, different experiences of different physicians, and availability of resources. Second, there was no information on how players with either AAIS or PAIS were treated, and if they had associated arthroscopic findings if they underwent surgical treatment. The type of impingement, whether bony or soft tissue, was also not recorded. Third, we did not capture data on the players’ medical history, such as ankle instability or fractures. Fourth, AAIS led to time loss in our study compared to PAIS. This might also be because AAIS more frequently requires surgery. Fifth, we acknowledge the limitation of our injury definition that could clarify why PAIS was a more frequent cause of time loss in professional football, while we are unaware of the total prevalence of symptomatic ankle impingement in the cohort, since many symptomatic AAIS and PAIS may not be captured when using a time loss injury definition given that players may have symptoms but are not taken out of play. Sixth, even though the study sample of professional players was large, some sub-analyses were limited by a small number of injuries and there is a risk of type 2 error. Finally, we utilized in-season time loss as an indicator of the severity of the injury. Consequently, injuries with off-season rest, treatment, or surgery might be missed.
Conclusion
The overall incidence of symptomatic ankle impingement in the current study was 0.03 injuries per 1000 h and resulted in an injury burden of 0.4 days absence per 1000 h. PAIS was 1.7 times more frequent than AAIS, but days of absence was significantly greater for AAIS in comparison to PAIS and AAIS had a higher re-injury rate than PAIS.
References
Andersson JK, Bengtsson H, Waldén M, Karlsson J, Ekstrand J (2021) Hand, wrist, and forearm injuries in male professional soccer players: a prospective cohort study of 558 team-seasons from 2001–2002 to 2018–2019. Orthop J Sports Med 9(1):232–239
Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF et al (2020) International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med 54(7):372–389
Brodsky AE, Khalil MA (1987) Talar compression syndrome. Foot Ankle 7(6):338–344
Calder JD, Sexton SA, Pearce CJ (2010) Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med 38(1):120–124
Feria-Arias E, Boukhemis K, Kreulen C, Giza E (2018) Foot and ankle injuries in soccer. Am J Orthop 47(10):23–28
Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J et al (2006) Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med 16(2):97–106
Hägglund M, Waldén M, Bahr R, Ekstrand J (2005) Methods for epidemiological study of injuries to professional football players: developing the UEFA model. Br J Sports Med 39(6):340–346
Hayashi D, Roemer FW, D’Hooghe P, Guermazi A (2015) Posterior ankle impingement in athletes: pathogenesis, imaging features and differential diagnoses. Eur J Radiol 84(11):2231–2241
Junge A, Dvorak J (2004) Soccer injuries: a review on incidence and prevention. Sports Med 34(13):929–938
Kudaş S, Dönmez G, Işık Ç, Çelebi M, Çay N, Bozkurt M (2016) Posterior ankle impingement syndrome in football players: case series of 26 elite athletes. Acta Orthop Traumatol Turc 50(6):649–654
Lavery KP, McHale KJ, Rossy WH, Theodore G (2016) Ankle impingement. J Orthop Surg Res 11(1):97
López Valerio V, Seijas R, Alvarez P, Ares O, Steinbacher G, Sallent A et al (2015) Endoscopic repair of posterior ankle impingement syndrome due to os trigonum in soccer players. Foot Ankle Int 36(1):70–74
Lubberts B, D’Hooghe P, Bengtsson H, DiGiovanni CW, Calder J, Ekstrand J (2019) Epidemiology and return to play following isolated syndesmotic injuries of the ankle: a prospective cohort study of 3677 male professional footballers in the UEFA Elite Club Injury Study. Br J Sports Med 53(15):959–964
Massada JL (1991) Ankle overuse injuries in soccer players. Morphological adaptation of the talus in the anterior impingement. J Sports Med Phys Fitness 31(3):447–451
McMurray TP (1950) Footballer’s ankle. J Bone Joint Surg 32:68–69
Morris LH (1943) Report of cases of athlete’s ankle. J Bone Joint Surg 25:220–224
Murawski CD, Kennedy JG (2010) Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med 38(10):2017–2024
Oztekin HH, Boya H, Ozcan O, Zeren B, Pinar P (2009) Foot and ankle injuries and time lost from play in professional soccer players. Foot (Edinb) 19(1):22–28
Rae K, Orchard J (2007) The orchard sports injury classification system (OSICS) version 10. Clin J Sport Med 17(3):201–204
Ribbans WJ, Ribbans HA, Cruickshank JA, Wood EV (2015) The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg 21(1):1–10
Ross KA, Murawski CD, Smyth NA, Zwiers R, Wiegerinck JI, van Bergen CJ et al (2017) Current concepts review: arthroscopic treatment of anterior ankle impingement. Foot Ankle Surg 23(1):1–8
Shiota J, Momma D, Yamaguchi T, Iwasaki N (2020) Long-term stress distribution patterns across the ankle joint in soccer players: a computed tomography osteoabsorptiometry study. Orthop J Sports Med 8(11):84–90
Smyth NA, Zwiers R, Wiegerinck JI, Hannon CP, Murawski CD, van Dijk CN et al (2014) Posterior hindfoot arthroscopy: a review. Am J Sports Med 42(1):225–234
Tol JL, van Dijk CN (2006) Anterior ankle impingement. Foot Ankle Clin 11(2):297–310
Tol JL, Slim E, van Soest AJ, van Dijk CN (2002) The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med 30(1):45–50
van Dijk CN, de Leeuw PA, Scholten PE (2009) Hindfoot endoscopy for posterior ankle impingement. Surgical technique. J Bone Joint Surg Am 91(Suppl 2):287–298
Waldén M, Hägglund M, Ekstrand J (2005) UEFA Champions League study: a prospective study of injuries in professional football during the 2001–2002 season. Br J Sports Med 39(8):542–546
Waldén M, Hägglund M, Ekstrand J (2013) Time-trends and circumstances surrounding ankle injuries in men’s professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med 47(12):748–753
Walls RJ, Ross KA, Fraser EJ, Hodgkins CW, Smyth NA, Egan CJ et al (2016) Football injuries of the ankle: a review of injury mechanisms, diagnosis and management. World J Orthop 7(1):8–19
Zekry M, Shahban SA, El Gamal T, Platt S (2019) A literature review of the complications following anterior and posterior ankle arthroscopy. Foot Ankle Surg 25(5):553–558
Acknowledgements
The authors would like to thank Dr. Ahmed Attia and Dr. Theodorakys Marin for their valued support to the paper.
Funding
Open Access funding provided by the Qatar National Library. All authors confirm to have received no funding related to this paper.
Author information
Authors and Affiliations
Contributions
PD’H: principal investigator, data acquisition, data analysis, and writing. MW: data analysis and review. MH: data analysis and review. HB: data acquisition, statistical analysis, and review. JE: data acquisition, data analysis, and review.
Corresponding author
Ethics declarations
Conflict of interest
All authors confirm to have no conflict of interest to the content of this paper.
Ethical approval
Individual ethical approval was also obtained from the ethical review authorities in Denmark, Norway and Sweden (#01-062, #M240-09, and #S-06188).
Informed consent
Written informed consents have been collected from all participating players in accordance with the Declaration of Helsinki. The general study protocol was reviewed and approved by the UEFA Football Development Division and the UEFA Medical Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
D’Hooghe, P., Waldén, M., Hägglund, M. et al. Anterior ankle impingment syndrome is less frequent, but associated with a longer absence and higher re-injury rate compared to posterior syndrome: a prospective cohort study of 6754 male professional soccer players. Knee Surg Sports Traumatol Arthrosc 30, 4262–4269 (2022). https://doi.org/10.1007/s00167-022-07004-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07004-4