Abstract
Purpose
Subacromial impingement syndrome (SIS) is associated with low self-reported shoulder function, impairments in shoulder strength and range of motion (ROM), and pain. It is not known how the symptomatology associated with SIS is reflected in the choice of treatment. This study compares self-reported shoulder function, shoulder strength, ROM, and pain in patients with SIS considered candidates and non-candidates for subacromial decompression (SAD).
Method
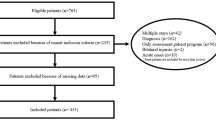
Self-reported shoulder function (Q-DASH and SPADI), maximum isometric muscle strength in shoulder abduction (Abd-strength) and external rotation (ER-strength), active abduction ROM (Abd-ROM) and passive internal rotation ROM (IR-ROM) were measured in a consecutive cohort of patients with SIS referred to an orthopedic outpatient clinic. Additionally, pain during each test and pain levels during the last week were reported. Patients were categorized as candidates or non-candidates for SAD based on their consultation with an orthopedic specialist blinded to test results and self-reported shoulder function. All outcomes and age, gender, weight and duration of symptoms were compared using the unpaired t test or Mann–Whitney’s U test as appropriate.
Results
One-hundred and fifty-seven patients were included. 25 patients were candidates for SAD, while 132 were not. SAD candidates had significantly lower Abd-ROM (87° vs. 112°, p = 0.011, effect size = 0. 15) and IR-ROM (114° vs. 123°, p = 0.026, effect size = 0.58) additional to higher pain during test of Abd-strength (5.3 vs. 3.7, p = 0.02, effect size = 0.21). No other differences were found between the groups.
Conclusion
A decrease in abduction and internal rotation range of motion, and increased pain during maximal abduction strength effort are associated with being considered a candidate for subacromial decompression, while self-reported shoulder function, pain during the last week, and rotator cuff strength are not. As SAD candidates primarily differentiates from non-candidates by having more pronounced ROM deficits, it might be important to address ROM in pre- and postsurgical evaluations, but as the overall differences between the two groups seem minor, the relation between impairments and the choice of treatment needs further clarification.
Level of evidence
IV.
Similar content being viewed by others
Abbreviations
- SIS:
-
Subacromial impingement syndrome
- ROM:
-
Range of motion
- SAD:
-
Subacromial decompression
- Q-DASH:
-
Quick version of the disabilities of the arm, shoulder and hand outcome measure
- SPADI:
-
Shoulder pain and disability index
- Abd-strength:
-
Maximum isometric muscle strength in shoulder abduction
- ER-strength:
-
Maximum isometric muscle strength in shoulder external rotation
- Abd-ROM:
-
Active abduction range of motion
- IR-ROM:
-
Passive internal rotation range of motion
- NPRS:
-
Numeric pain rating scale
- CI:
-
Confidence interval
- Abd-ROMPain :
-
Pain during test of Abd-ROM
- NPRS-Max/-Min/-Avg:
-
Maximum/minimum/average shoulder pain during the last week
- NPRS-Pre:
-
Present shoulder pain.
References
van der Windt DA, Koes BW, de Jong BA, Bouter LM (1995) Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 54:959–964
Östör AJK, Richards CA, Prevost AT, Speed CA, Hazleman BL (2005) Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology 44:800–805
Chipchase LS, Connor DAO, Hons B, Costi JJ, Hons BE, Krishnan J (2000) Shoulder impingement syndrome: preoperative health status. J Shoulder Elbow Surg 9:12–15
Macdermid JC, Ramos J, Drosdowech D, Faber K (2004) The impact of rotator cuff pathology on isometric and isokinetic strength, function, and quality of life. J Shoulder Elbow Surg 13:593–598
Celik D, Sirmen B, Demirhan M (2011) The relationship of muscle strength and pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc 45:79–84
Roach KE, Budiman-Mak E, Songsiridej NLY (1991) Development of a shoulder pain and disability index. Arthritis Care Res 4:143–149
Tyler TF, Nahow RC, Nicholas SJ, Mchugh MP, York N (2005) Quantifying shoulder rotation weakness in patients with shoulder impingement. J Shoulder Elb Surg 14:570–574
Özlem Erol MD, Levent Özcakar MD, Reyhan Celiker M (2008) Shoulder rotator strength in patients with stage I-II subacromial impingement: relationship to pain, disability, and quality of life. J Shoulder Elbow Surg 17:893–897
Engebretsen K, Grotle M, Bautz-Holter E, Ekeberg OM, Brox JI (2010) Determinants of the shoulder pain and disability index in patients with subacromial shoulder pain. BMC Musculoskelet Disord 11:218
Tyler TF, Nicholas SJ, Roy T, Gleim GW (2000) Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med 28:668–673
Johansson K, Öberg B, Adolfsson L, Foldevi M (2002) A combination of systematic review and clinicians’ beliefs in interventions for subacromial pain. Br J Gen Pract 52:145–152
Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN (2008) Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008:CD005619
Jaeger M, Berndt T, Rühmann O, Lerch S (2016) Patients with impingement syndrome with and without rotator cuff tears do well 20 years after arthroscopic subacromial decompression. Arthroscopy 32:409–415
Farfaras S, Sernert N, Hallström E, Kartus J (2016) Comparison of open acromioplasty, arthroscopic acromioplasty and physiotherapy in patients with subacromial impingement syndrome: a prospective randomised study. Knee Surg Sport Traumatol Arthrosc 24:2181–2191
Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, Aronen P, Konttinen YT, Malmivaara A, Rousi T (2009) Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg Br 91:1326–1334
Vandenbroucke JP, Elm E, Von Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, Initiative S (2014) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg 12:1500–1524
Clausen MB, Witten A, Holm K, Christensen KB, Attrup ML, Hölmich P, Thorborg K (2017) Glenohumeral and scapulothoracic strength impairments exists in patients with subacromial impingement, but these are not reflected in the shoulder pain and disability index. BMC Musculoskelet Disord 18:1–10
Christiansen DH, Andersen JH, Haahr JP (2013) Cross-cultural adaption and measurement properties of the Danish version of the shoulder pain and disability index. Clin Rehabil 27:355–360
Gummesson C, Ward MM, Atroshi I (2006) The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 7:44
Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, Wright AA (2012) Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med 46:964–978
Michener LA, Walsworth MK, Doukas WC, Murphy KP (2009) Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 90:1898–1903
Schønnemann JO, Eggers J (2016) Validation of the danish version of the quick-disabilities of arm, shoulder and hand questionnaire. Dan Med J 63:A5306
Çelik D, Dirican A, Baltaci G (2012) Intrarater reliability of assessing strength of the shoulder and scapular muscles. J Sport Rehabil 29:1–5
Hayes K, Walton JR, Szomor ZL, Murrell GA (2002) Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg 11:33–39
Kolber MJ, Vega F, Widmayer K, Cheng M-SS (2011) The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother Theory Pract 27:176–184
Lunden JB, Muffenbier M, Giveans MR, Cieminski CJ (2010) Reliability of shoulder internal rotation passive range of motion measurements in the supine versus sidelying position. J Orthop Sports Phys Ther 40:589–594
Green S, Buchbinder R, Hetrick S (2003) Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev 2003:CD004258
Roddey T, Cook K, O’Malley K, Gartsman G (2005) The relationship among strength and mobility measures and self-report outcome scores in persons after rotator cuff repair surgery: impairment measures are not enough. J Shoulder Elbow Surg 14:95–98
Danish Health Authority (2016) National clinical guideline on diagnostics and treatment of patients with selected shoulder conditions. Danish Health Authority, Copenhagen
Acknowledgements
The authors would like to thank Peter Andreas Rothe, Jens Langermann and Kika Holm for assisting with the data collection.
Funding
The study was funded by University College Copenhagen; Sports Orthopedic Research Center-Copenhagen, Department of Orthopedic Surgery, Copenhagen University Hospital, Amager-Hvidovre, Denmark.
Author information
Authors and Affiliations
Contributions
AW contributed to the design of the study, and acquisition, analysis and interpretation of data. MBC contributed with the acquisition and interpretation of data. MLA contributed with the acquisition of data. KT and PH contributed to the design of the study and interpretation of data. All authors have contributed to the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare to have no financial or non-financial competing interests.
Ethical approval
The project was approved by the Danish Data Protection Agency, and has also been evaluated by the Capitol Region Committee on Health Research Ethics in Denmark, where it was evaluated as not requiring formal ethical approval (H-3-2013-FSP29).
Rights and permissions
About this article
Cite this article
Witten, A., Clausen, M.B., Thorborg, K. et al. Patients who are candidates for subacromial decompression have more pronounced range of motion deficits, but do not differ in self-reported shoulder function, strength or pain compared to non-candidates. Knee Surg Sports Traumatol Arthrosc 26, 2505–2511 (2018). https://doi.org/10.1007/s00167-018-4894-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4894-6