Abstract
Purpose
Leakage of oral secretions past endotracheal tubes (ETT) has been implicated in ventilator associated pneumonia. The aim of this bench study was to compare the ability of current generation ETT cuffs to prevent fluid leakage and to determine the specific mechanical ventilator settings that affect movement of fluid across an inflated ETT cuff.
Methods
Using a 2.3-cm internal diameter (ID) tracheal model and simulated ventilatory support, we evaluated the impact of cuff pressure (20 and 30 cmH2O), positive end-expiratory pressure/continuous positive airway pressure (PEEP/CPAP, 0–15 cmH2O), peak inspiratory pressure (PIP, 15–45 cmH2O), and mode of ventilation (volume control, volume assist/control, pressure control, pressure assist/control, and CPAP) on leakage of fluid past the ETT cuffs of 16 ETTs. The tracheal model was configured in the vertical position with 35 ml of vitaminwater® on top of the inflated ETT cuff and mechanically ventilated. Fluid leakage past the cuff was determined by calculating the volume change in the tracheal model after each 30-min ventilation period. Initially five 8.0-mm-ID ETTs of each manufacturer type were evaluated at baseline ventilator settings. Tubes allowing a consistent leak within two SD of the mean leakage for the five tubes were numbered in consecutive order. A single tube from this group was then randomly selected for detailed evaluation.
Results
Cuff leakage varied among ETT types (p < 0.0001); median leak volume 6.0 ml (0.6–15.1) across all tubes under all conditions. Cuff leakage was inversely related to PEEP level, cuff pressure, and PIP except when PEEP was set at 15 cmH2O (all p < 0.0001). In addition, cuff leak varied among modes (p = 0.035).
Conclusion
Cuff leakage varies greatly among ETT types and is affected by cuff pressure, PEEP, PIP, and mode.
Similar content being viewed by others
Introduction
Ventilator associated pneumonia (VAP) results in increased cost of hospitalization, length of mechanical ventilation, ICU stay, morbidity, and mortality [1]. Some have attributed mortalities from 13 to 55% as a direct result of VAP [2]. By the third day of endotracheal intubation and mechanical ventilation 70% of patients’ airways are colonized [3]. Ventilator bundles have been promoted as a way of reducing VAP [4]. These ventilator bundles recommend among other things proper cuff inflation techniques, maintaining the head of the bed elevated at more than 30°, frequent and appropriate oral hygiene, increased use of noninvasive ventilation, and rapid weaning from ventilatory support [5, 6]. However, little emphasis has been placed on the performance of the endotracheal tube (ETT) cuff and the impact of ventilator settings on movement of fluid past the cuff of the ETT [7, 8].
Manufacturers of ETT have engineered cuffs to provide enough cuff material to ensure that the cuff is “passively” draped along the tracheal wall requiring low cuff inflation pressures to avoid air leak and lessen complications as a result of cuff pressure occluding mucosal capillary blood flow [9]. However, as a result of the large cuff volume, low cuff pressure design, leakage of oral secretions past inflated ETT cuffs is well documented both in vitro and in vivo [7, 8]. The primary cause of leakage is the development of folds in the cuff providing channels for secretions to move past the cuff by capillary action [10, 11]. These folds are developed as a result of the cuff diameter, wall thickness, and intra-cuff pressure [10, 12]. Recently, some manufacturers have introduced new cuff designs, using ultrathin polyurethane and alternate shapes to reduce the movement of fluid past the inflated cuff [7, 10]. However, systematic evaluation of the performance of ETT cuffs manufactured by different companies remains to be performed.
The aims of this study were to compare the ability of current generation ETT cuffs to prevent fluid leakage and to determine the specific mechanical ventilator settings that affected movement of fluid across an inflated ETT cuff. We hypothesized that in a bench tracheal airway model cuff leakage would be affected by type of ETT, and that leakage would be indirectly related to cuff pressure, PEEP/CPAP level, and peak inspiratory pressure but unaffected by mode of ventilation.
Materials and methods
Model setup
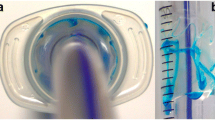
The tracheal model used was the same as that described by Young et al. [9]. It consisted of a silicone tube of 2.3-cm ID and 28 cm in length (Laerdal Medical silicone extension tubing, part number 871000) connected to a Michigan Instruments test lung allowing both controlled and spontaneous triggering of the ventilator attached to the endotracheal tube being evaluated [13] (Fig. 1). See online material for complete description.
Experimental setup. The silicone model tracheal was connected to a ring stand and maintained in a vertical position. The distal portion of the silicone trachea was connected to a rigid water trap which in turn was connected to a model lung (a two-chambered Michigan Instruments test lung). The proximal portion of the model was open to atmosphere, allowing for the insertion of each ETT evaluated. In order to simulate spontaneous breathing a ventilator was connected to the contralateral lung of the model. A lift bar was attached to simulate spontaneous breathing. That is ventilation of the contralateral lung resulted in the lift bar expanding the lung simulator creating a negative pressure triggering the patient ventilator
Endotracheal tube selection
Initially five 8.0-mm-ID ETTs of each manufacturer type (Table 1) were evaluated at baseline ventilator settings: pressure control mode, inspiratory pressure 20 cmH2O, PEEP 5 cmH2O, rate 20 breaths/min, and inspiratory time 1.0 s applied for 30 min. The ETT cuff was inflated to 20 cmH2O and 35 ml of fluid was placed on top of the inflated cuff. Tubes allowing a consistent leak within two standard deviations of the mean leakage for the five tubes were numbered in consecutive order. A single tube from this group was then randomly selected for detailed evaluation. The actual data presented in this study is the evaluation of the single tube selected as described above from each manufacturer.
Study protocol
Following cuff inflation 10 cmH2O CPAP was applied to the ETT–lung model system in order to prevent fluid from immediately leaking past the cuff. Once the pressure within the system stabilized, 35 ml of red-colored vitaminwater® (Glaceau, Whitestone, NY, USA; Revive flavor, density 1.016 g/ml) was placed above the cuff, creating a column of liquid, approximately 10 cm above the cuff. After establishment of the fluid column, the ventilator was immediately adjusted to one of the following modes: pressure control ventilation (PCV), pressure assist/control ventilation (PAC), volume control ventilation (VCV), and volume assist/control ventilation (VAC) and continuous positive airway pressure (CPAP). In each mode various tidal volumes/peak pressures and PEEP/CPAP levels were applied. See online material for precise settings of each mode.
A total of 64 independent evaluations were performed on each tube. Each mode and pressure evaluation was conducted for a 30-min period. The following parameters were recorded: airway pressure, initial height of the fluid level above the cuff, and final height of fluid above the cuff. Leak was defined as liquid that had leaked past the inflated cuff or had been forced out of the tracheal model during inspiration. Fluid level was determined by one of two investigators (RP and DF) and fluid level was always measured at the bottom of the meniscus at a stable end-expiratory pressure. Leakage volume was determined from the change in fluid height after correcting for volume displaced by the ETT. See online material for complete description.
Body temperature and pressure saturated (BTPS) evaluation
The two best performing ETT (tubes 1 and 12) and tube 2 selected from the next group of high performing tubes were further evaluated under BTPS conditions. The same tracheal/ventilator model was placed in one cube care tent within another. The space between tents was insulated by using blankets. The internal environment was heated by using a Bair Hugger® forced air warming unit set at 38°C (model 505, Augustine Medical, Eden Prairie, MN, USA). The relative humidity was kept at 100% by adding to the cube tent 25 l/min medical air heated and humidified at 39°C (Neptune, Teleflex) maintaining the cube tent 37°C. The model was allowed to stabilize for 1 h before each ETT was studied. Each ETT cuff was inflated to 30 cmH2O and the model was ventilated in the PA/C mode, PIP 35 cmH2O, PEEP 15 cmH2O, rate 20 breaths/min, and IT 1 s for a 6-h period.
Data analysis and statistics
All data are presented as mean ± standard deviation (SD) or median and interquartile range dependent on the distribution of the data. Data are grouped by ETT type, cuff pressure, PEEP level, PIP, and mode of ventilation. Comparisons were performed by the Kruskal–Wallis test followed by pairwise Mann–Whitney U tests (with correction for statistical significance) when significance differences were identified. Independent sample t tests were used for the initial evaluation of ETTs of each type. In addition, linear regressions were performed on the effects of PEEP and PIP on leak volume. SPSS statistical software (SPSS 15.0 for Windows, Chicago, IL, USA) was used. A p < 0.05 was considered significant in all comparisons.
Results
Results of the preliminary study identifying the specific ETTs of each type extensively studied are presented in the online material (Table A). With most manufacturer types little variability in leak existed among the five tubes and random selection of the study tube was from the total of five tubes from each manufacturer.
Figure 2 illustrates the results of the composite comparisons of all evaluations for each of the 16 tubes studied in which fluid was not forced out the top of the model during the evaluation. In some evaluations on select ETT, fluid was forced out of the top of the tracheal model (online material Table B). Since we were unable to differentiate the volume of fluid leaking across the cuff from the volume expelled from the system, we have eliminated these individual trials from the statistical analysis. Direct measurement of fluid leakage was impossible because any physical disturbance of the model resulted in more fluid leaking past the ETT cuff. All subsequent discussions address only those trials where no fluid was expelled from the top of the model.
Leakage of fluid by endotracheal tube type. Median and interquartile range of fluid leakage across all evaluations in which fluid was not forced out the top of the model during the evaluation for each ETT evaluated. Leakage differed among ETT types, p < 0.0001. *Leak less than or greater than all other tubes, p < 0.01. The largest leak was observed with the Sheridan/CF (Teleflex) tube (14.2 ml (2.07–22.85). The SealGuard tube from Covidien [median leak 0.3 ml (0.0–0.6)] and the Microcuff tube from Kimberly-Clark [median leak 0.0 ml (0.0–0.0)] had the lowest median leak. Tube identities are explained in Table 1
As noted (Fig. 2) there were large differences among ETT type, p < 0.0001. The median leak volume across all tubes was 6 ml (0.6–15.1). The single factor that had the greatest impact on leak past the ETT cuff was PEEP level, p < 0.0001. The greater the PEEP level, the smaller the leak (Fig. 3). Figure 4 illustrates the impact of peak inspiratory pressure on leak volume. At a constant PEEP level, PIP and leak volume were inversely related, p < 0.0001 except when PEEP was set at 15 cmH2O. The leak volume was lower 4.4 ml (0.3–13.2) at 30 cmH2O cuff pressure than at 20 cmH2O cuff pressure, 7.8 ml (0.617.4) (p = 0.005) (online material Fig. A). The relationship between PEEP and leak and PIP and leak were weak. The linear regression for the effect of PEEP on leak had a p < 0.001 but r 2 of 0.31 with a slope of −1.37 and an intercept of 22.49. PIP had less of an effect on leak, p < 0.001, r 2 0.19, slope −0.34, and an intercept of 18.12. Combining PIP with PEEP did not affect r 2, still 0.32.
Leakage of fluid by peak inspiratory pressure. Median and interquartile range of fluid leakage for all evaluations in which fluid was not forced out the top of the model during the evaluation for all ETTs collapsed and sorted by peak inspiratory pressure/PEEP (PIP/PEEP) level. At a PEEP of 5 cmH2O, peak inspiratory pressure (PIP) of 25 cmH2O differed from PIP of 5 and 15 cmH2O; and at a PEEP of 10 cmH2O, PIP of 30 and 40 cmH2O both differed from PIP of 10 and 20 cmH2O. *p < 0.0001
There was a small but significant effect of mode on leak (p = 0.035) with the greatest leak occurring during PCV [8 ml (0.9–17.5)] and the least leak during PA/C [3.8 ml (0.6–12.5)]. PCV was also different from VA/C (6 ml (0.0–14.5) C (p = 0.027) (online material Fig. B).
The BTPS evaluation of ETT 1, 2, and 12 all produced the same results. No fluid whatsoever leaked past the cuffs of any of these tubes over the 6-h evaluation period.
Discussion
The primary findings of this lung model study can be summarized as the following: (1) The ability of the cuffs of the ETT evaluated to prevent leakage of fluid is highly variable. (2) The single ventilator parameter that contributed to the greatest reduction in fluid leakage was PEEP. (3) Peak inspiratory pressure is also inversely related to fluid leakage except at a PEEP of 15 cmH2O. And (4) cuff pressure and mode of ventilation do affect leakage past the ETT but not to the extent observed with ETT type, PEEP, and peak inspiratory pressure.
The single most important factor affecting the development of VAP may quite possibly be the ETT [14]. As we have shown in our current study most ETTs currently on the market are incapable of preventing large quantities of fluid from leaking past their inflated cuffs. The primary reason for this fluid leak is the development of channels when these cuffs are inflated [7–10]. When channels are present in the folds of cuffs fluid from above the cuff moves by capillary action past the cuff into the patients’ lower airway [10, 11]. This movement can be reduced by the presence of PEEP, proper cuff inflation, and high airway pressure. However, under the conditions tested in this lung model study most tubes still allowed leakage. As noted in Fig. 2, two tubes dramatically outperformed the other tubes evaluated. Both of these tubes have alternate cuff designs and their cuffs are made from ultrathin polyurethane. One has a cylindrical shape and the other an inverted pear shape. In addition, the inflated length of these tubes’ cuffs exceeded that of the other tubes tested by at least about 3 mm but their inflation diameter was less than that of many tubes (Table 1). Surface area of cuff to trachea contact combined with the ultrathin polyurethane material may be the primary reason for reduced leakage. Since the walls of these polyurethane cuffs are so thin, it appears that when they do fold, they do not form large open channels as occurs with standard cuffs. Such features are likely to account for their ability to prevent leakage [7, 10]. It is important to note that tube number 5 which had the greatest leak also had the smallest inflation diameter at 20 cmH2O cuff pressure, less than the ID of the tracheal model by about 0.5 mm (Table A). In addition, as noted in Table B some ETTs under specific PIP/PEEP settings allowed fluid to be expelled from the tracheal model. We have assumed this is a result of large cuff leaks but we were not able to separate fluid expelled from fluid leaked in these situations. This should be taken into consideration when evaluating the performance of these ETTs.
Cuff pressure
Cuff inflation pressure is recommended to be between 20 and 30 cmH2O [5, 15] by some and 25–30 cmH2O by others [7, 11]. As is clear from Fig. 5 this is insufficient pressure to prevent leakage of fluid past most cuffs of ETTs in this study. However, the application of higher pressure is of concern because of tracheal injury resulting from the obstruction of blood flow in the tracheal mucosal wall [16]. It seems most reasonable to routinely apply the highest cuff pressure that is not associated with tracheal injury to minimize the amount of fluid moving past the ETT cuff. It is also clear that we cannot depend on proper cuff pressure to prevent aspiration; newer and more effective cuffs must become available if we are to prevent channeling of fluid past the cuff.
PEEP
In our lung model, after the actual ETT, PEEP was the most effective maneuver reducing fluid leak across the ETT cuff (Fig. 3); however, linear regression indicated it only accounted for 31% of the leak. We believe that PEEP counteracted the hydrostatic pressure of the fluid preventing fluid movement. This concept is not new; Janson and Poulton [17] first described the effect of PEEP on leakage of fluid past ETTs using a tracheal model. More recently, both Lucangelo et al. [7] and Manzano et al. [8] demonstrated the beneficial effect of PEEP on aspiration or VAP. Manzano et al. randomized 150 patients to zero PEEP and to 5–8 cmH2O PEEP and found that those receiving PEEP had a lower incidence of VAP (25% control group and 9.45% in the PEEP group, p < 0.017).
Peak airway pressure
High PIP creates a hydrostatic barrier to fluid movement during inspiration but it is the application of PEEP during expiration that may be the predominant factor preventing leakage since generally expiratory time is about twice as long as inspiratory time. At 15 cmH2O PEEP the effect of PEEP on fluid leakage was so great that increasing PIP did not additionally affect fluid leakage.
Mode of ventilation
Mode of ventilation did affect leakage of fluid past the ETT cuff contrary to our hypothesis, although the differences were small. The greatest movement of fluid occurred during pressure ventilation most likely because for a given tidal volume PIP is lower during pressure ventilation than volume ventilation.
BTPS
When the best performing tubes were evaluated at BTPS at the best cuff pressure (30 cmH2O), PEEP level (15 cmH2O), and PIP level (35 cmH2O) during the PA/C mode no leak was observed for any of these tubes. Thus, although this was not a patient, it appears that fluid movement past an ETT cuff can be totally stopped under optimal conditions.
Comparison to others studies
The first to study leakage past ETT using the model we employed was Young et al. [18]. They demonstrated that even at a cuff pressure of 60 cmH2O leakage of about 0.03–0.15 ml/s occurs depending on the height of the column of fluid above the cuff. Young et al. [19] compared two ETTs with standard large volume low pressure cuffs to a cuff they designed; their novel cuff did not leak. Using Young’s model Asai and Shingu [20] compared four ETTs at cuff pressures of 20–40 cmH2O during volume controlled ventilation with zero PEEP. All cuffs leaked at least 2.0 ml at the 40 cmH2O cuff pressure and between 5 and 10 ml at the 20 cmH20 cuff pressure setting.
More recently, Young et al. [9] compared a high volume low pressure (HVLP) to a low volume low pressure (LVLP) cuff in his tracheal model, a swine tracheal model, and in patients. In all evaluations the HVLP cuff leaked excessively; however, in neither of the models nor in patients were leaks observed with the LVLP cuff. Dullenkopf et al. [10] compared the Microcuff to five other standard ETTs. They found that fluid leakage occurred even at 60 cmH2O cuff pressure with standard ETT cuffs but with the Microcuff fluid leakage could be prevented by cuff pressures of 30 cmH2O or less. Zanella et al. [21] compared a prototype cuff with four standard ETT cuffs. The prototype cuff outperformed the other four cuffs. Finally, Poelaert et al. [22], in a prospective randomized controlled trial, demonstrated a decrease in early postoperative pneumonia in patients intubated with an ultrathin polyurethane cuff compared to patients intubated with a standard polyvinyl chloride cuff.
Limitations
The primary limitations of this study are that it was not performed on patients and the model trachea used was not an animal or human trachea. In addition the diameter of the tracheal model was large, 2.3 cm, potentially exceeding that of most female patients and in some evaluations we were not able to separate the volume of fluid expelled from the tracheal model from that leaked across the ETT cuff (Table B). Secondly, the magnitude of the effects must be questioned since the study design was a worst-case scenario. The hydrostatic pressure established above the cuff most likely exceeded that observed in the average critically ill patient’s airway. Most reports indicate that the volume of fluid normally sitting on top of cuffs is a few milliliters (3–6 ml) [23]. In addition the viscosity and density of normal oral secretions is much higher than the vitaminwater® that we used in this experiment. Thirdly, the evaluation of each condition was only conducted for a 30-min period. In actual clinical practice we would expect the leakage past any of these cuffs to be less then found in this study.
Conclusion
Most ETT cuffs currently in use are incapable of preventing fluid leakage in our tracheal model. However, fluid leakage was significantly minimized with the use of ultrathin-walled cuffs. Among the factors affecting leakage, PEEP had the greatest effect followed by PIP, cuff pressure, and then ventilator mode.
References
Heyland D, Cook D, Griffith L, Keene SP, Brun-Buisson (1999) The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. Am J Respir Crit Care Med 159:1249–1256
Petring O, Adelhoj B, Jensen B, Pederson NO, Lomholt N (1986) Prevention of silent aspiration due to leaks around cuffs of endotracheal tubes. Anesth Analg 65:777–780
Durairji L, Mohamed Z, Launspach JL, Ashare A, Choi JY, Rajagopal S, Doern GV, Zabner J (2009) Patterns and density of early tracheal colonization in intensive care unit patients. J Crit Care 24:114–121
Blamoun J, Alfakir M, Rella M, Wojcik JM, Solis RA, Anees Klan M, Debari VA (2009) Efficacy of an expanded ventilator bundle for the reduction of ventilator-associated pneumonia in the medical intensive care unit. Am J Infect Cont 37:172–175
Coffin S, Klompas M, Classen D, Arias KM, Podgorny K, Anderson DJ, Burstin H, Calfee DP, Dubberke ER, Fraser V, Gerding DN, Griffen EA, Gross P, Kaye KS, Lo E, Marscall J, Mermel LA, Nicolle L, Pegues DA, Perl TM, Saint S, Salgado CD, Weinstein RA, Wise R, Yokoe DS (2008) Strategies to prevent ventilator-associated pneumonia in acute care hospitals. Infect Cont Hosp Epidemiol 29:31–40
Torres A, Ewig S, Lode H, Carlet J, For the European HAP working group (2009) Defining, treating and preventing hospital acquired pneumonia: European perspective. Intensive Care Med 35:9–29
Lucangelo U, Zin W, Antonaglia V, Petrucci L, Viviani M, Buscema G, Borelli M, Berlot G (2008) Effect of positive expiratory pressure and type of tracheal cuff on the incidence of aspiration in mechanically ventilated patients in an intensive care unit. Crit Care Med 36:409–413
Manzano F, Fernandez-Mondejar E, Colmenero M, Poatos ME, Rivera R, Machado J, Catalan I, Artigas A (2008) Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemia patients. Crit Care Med 36:2225–2231
Young P, Pakeerathan S, Blunt M, Poyatos ME, Rivera R, Machado J, Catalan I, Artigus A (2006) A low-volume, low-pressure tracheal tube cuff reduces pulmonary aspiration. Crit Care Med 34:632–639
Dullenkopf A, Gerber A, Weiss M (2003) Fluid leakage past tracheal tube cuffs: evaluation of the new Microcuff endotracheal tube. Intensive Care Med 29:1849–1853
Seegobin R, van Hasselt G (1986) Aspiration beyond endotracheal cuffs. Can Anaesth Soc J 33:273–279
Ozkurt S, Sungurtekin H, Aydemir N, Atalay H, Zencir M, Baser S, Kaleli I (2007) Ventilator associated pneumonia: retrospective results in an intensive care unit. J Internet Gastroenterol vol 5. http://www.ispub.com/journal/the_internet_journal_of_gastroenterology/volume_5_number_2_13/article/ventilator_associated_pneumonia_retrospective_results_in_an_intensive_care_unit.html. Accessed 3 Jan 2010
Bigatello L, Nishimura M, Imanaka H, Hess D, Kimball W, Kacmarek RM (1997) Unloading of the work of breathing by proportional assist ventilation in a lung model. Crit Care Med 25:267–272
Hess D (2000) Noninvasive positive-pressure ventilation and ventilator-associated pneumonia. Respir Care 50:924–931
Rello J, Sonora R, Jubert P, Artigus A, Rue A, Valles J (1996) Pneumonia in intubated patients:role of respiratory airway care. Am J Respir Crit Med 154:111–115
Bernhard W, Cotrell J, Sivakumaran C (1979) Adjustment of intracuff pressure to prevent aspiration. Anesthesiology 50:363–366
Janson B, Poulton T (1986) Does peep reduce the incidence of aspiration around endotracheal tubes? Can Anaesth Soc J 33:157–161
Young P, Rollinson M, Downward G, Henderson S (1997) Leakage of fluid past the tracheal tube cuff in a benchtop model. Brit J Anesth 78:557–562
Young P, Ridley S, Downward G (1998) Evaluation of a new design of tracheal tube cuff to prevent leakage of fluid to the lungs. Brit J Anaesth 80:796–799
Asai T, Shingu K (2001) Leakage of fluid around high-volume, low-pressure cuffs: a comparison of four tracheal tubes. Anaesthesia 56:38–42
Zanella A, Cressoni M, Epp M, Stylianou K, Kolobow T (2008) A double-layer tracheal tube cuff designed to prevent leakage: a bench-top study. Intensive Care Med 34:1145–1149
Poelaert J, Depuydt P, De Wolf A, Van de Velde S, Herck I (2008) Polyurethane cuffed endotrachea; tubes to prevent early postoperative pneumonia after cardiac surgery: a pilot study. J Thorac Cardiovasc Surg 135:771–776
Nseir S, Brisson H, Marquette C-H, Chaud P, Di Pompeo C, Diarra M, Durocher A (2009) Variations in endotracheal cuff pressure in intubated critically ill patients: prevalence and risk factors. Eur J Anesthesiol 26:229–234
Acknowledgments
The authors would like to thank Edward Bittner MD, PhD for his gracious assistance with the statistical analysis. This project was funded by a gift from Covidien, Carlsbad, CA, USA. Robert M Kacmarek has received research grants from Covidien, Hamilton, General Electric, Newport, and Drager; honorarium for lecturing from Covidien, Hamilton, and Maquet; and is a consultant for Newport and KCI.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pitts, R., Fisher, D., Sulemanji, D. et al. Variables affecting leakage past endotracheal tube cuffs: a bench study. Intensive Care Med 36, 2066–2073 (2010). https://doi.org/10.1007/s00134-010-2048-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2048-5