Abstract
Objective
Airway pressure limitation is now a largely accepted strategy in adult respiratory distress syndrome (ARDS) patients; however, some debate persists about the exact level of plateau pressure which can be safely used. The objective of the present study was to examine if the echocardiographic evaluation of right ventricular function performed in ARDS may help to answer to this question.
Design and patients
For more than 20 years, we have regularly monitored right ventricular function by echocardiography in ARDS patients, during two different periods, a first (1980–1992) where airway pressure was not limited, and a second (1993–2006) where airway pressure was limited. By pooling our data, we can observe the effect of a large range of plateau pressure upon mortality rate and incidence of acute cor pulmonale.
Results
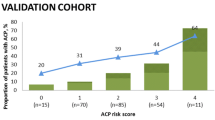
In this whole group of 352 ARDS patients, mortality rate and incidence of cor pulmonale were 80 and 56%, respectively, when plateau pressure was > 35 cmH2O; 42 and 32%, respectively, when plateau pressure was between 27 and 35 cmH2O; and 30 and 13%, respectively, when plateau pressure was < 27 cmH2O. Moreover, a clear interaction between plateau pressure and cor pulmonale was evidenced: whereas the odd ratio of dying for an increase in plateau pressure from 18–26 to 27–35 cm H2O in patients without cor pulmonale was 1.05 (p = 0.635), it was 3.32 in patients with cor pulmonale (p < 0.034).
Conclusion
We hypothesize that monitoring of right ventricular function by echocardiography at bedside might help to control the safety of plateau pressure used in ARDS.


Similar content being viewed by others
References
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28:596–608
Webb H, Tierney D (1974) Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressure. Protection by positive end-expiratory pressure. Am Rev Respir D 110:556–565
Dreyfuss D, Basset G, Soler P, Saumon G (1985) Intermittent positive-pressure hyperventilation with high inflation pressures produces pulmonary microvascular injury in rats. Am Rev Respir D 132:880–884
Hickling K, Henderson S, Jackson R (1990) Low mortality associated with low volume/pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 16:372–377
Whittenberger J, McGregor M, Berglund E, Borst H (1960) Influence of state of inflation of the lung on pulmonary vascular resistance. J Appl Physiol 15:878–882
Morgan B, Martin W, Hornbein T, Crowford E, Guntheroth W (1966) Hemodynamic effects of intermittent positive pressure respiration. Anesthesiology 27:584–590
Howell J, Permutt S, Proctor D, Riley R (1961) Effect of inflation of the lung on different parts of the pulmonary vascular bed. J Appl Physiol 16:71–76
Zapol W, Snider M (1977) Pulmonary hypertension in severe acute respiratory failure. N Engl J Med 296:476–480
Jardin F, Gurdjian F, Fouilladieu JL, Goudot B, Margairaz A (1979) Pulmonary and systemic hemodynamic disorders in adult respiratory distress syndrome. Intensive Care Med 5:127–133
Jardin F, Gueret P, Dubourg O, Farcot JC, Margairaz A, Bourdarias JP (1985) Two-dimensional echocardiographic evaluation of right ventricular size and contractility in acute respiratory failure. Crit Care Med 13:952–956
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111:209–217
Squara P, Dhainaut JF, Artigas A, Carlet J and the European Collaborative ARDS Working Group (1998) Hemodynamic profile in severe ARDS: results of the European Collaborative ARDS Study. Intensive Care Med 24:1018–1028
Monchi M, Bellenfant F, Cariou A, Joly JM, Thebert D, Laurent I, Dhainaut JF, Brunet F (1998) Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 158:1076–1081
Slutsky A (1993) Mechanical ventilation. American College of Chest Physicians' Consensus Conference. Chest 104:1833–1859
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart T, Benito S, Epstein S, Apezteguia C, Nightingale P, Arroliga A, Tobin M (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation. A 28-Day International study. J Am Med Assoc 287:345–355
Hager D, Krishnan J, Hayden D, Bower R (2005) Tidal volume reduction in patients with acute lung injury when plateau pressure are not high. Am J Respir Crit Care Med 172:1241–1245
Ferguson N, Frutos-Vivar F, Esteban A, Anzueto A, Alia I, Bower G, Stewart T, Apezteguia C, Gonzales M, Soto L, Abroug F, Brochard L (2005) Airway pressure, tidal volume, and mortality in patients with acute respiratory distress syndrome. Crit Care Med 33:21–30
Eichacker P, Gerstenberger E, Banks S, Xizhong C, Natanson S (2002) Meta-analysis of acute lung injury and acute respiratory distress syndrome trials testing low tidal volumes. Am J Respir Crit Med 166:1510–1514
Page B, Vieillard-Baron A, Beauchet A, Aegerter P, Prin S, Jardin F (2003) Low stretch ventilation strategy in acute respiratory distress syndrome: eight years of clinical experience in a single center. Crit Care Med 31:765–769
Vieillard-Baron A, Schmitt JM, Beauchet A, Augarde R, Prin S, Page B, Jardin F (2001) Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications and prognosis. Crit Care Med 29:1551–1555
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Deans K, Minneci P, Cui X, Banks S, Natanson C, Eichaker P (2005) Mechanical ventilation in ARDS: one size does not fit all. Crit Care Med 33:1141–1144
Gattinoni L, Pesanti A (2005) The concept of “baby lung”. Intensive Care Med 31:776–784
Acknowledgements
We gratefully acknowledge E. Girou for performing the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jardin, F., Vieillard-Baron, A. Is there a safe plateau pressure in ARDS? The right heart only knows. Intensive Care Med 33, 444–447 (2007). https://doi.org/10.1007/s00134-007-0552-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0552-z