Abstract
Objectives
Critical illness increases the tendency to both coagulation and bleeding, complicating anticoagulation for continuous renal replacement therapy (CRRT). We analyzed strategies for anticoagulation in CRRT concerning implementation, efficacy and safety to provide evidence-based recommendations for clinical practice.
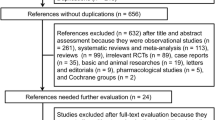
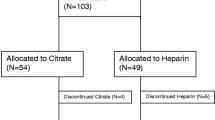
Methods
We carried out a systematic review of the literature published before June 2005. Studies were rated at five levels to create recommendation grades from A to E, A being the highest. Grades are labeled with minus if the study design was limited by size or comparability of groups. Data extracted were those on implementation, efficacy (circuit survival), safety (bleeding) and monitoring of anticoagulation.
Results
Due to the quality of the studies recommendation grades are low. If bleeding risk is not increased, unfractionated heparin (activated partial thromboplastin time, APTT, 1–1.4 times normal) or low molecular weight heparin (anti-Xa 0.25–0.35 IU/l) are recommended (grade E). If facilities are adequate, regional anticoagulation with citrate may be preferred (grade C). If bleeding risk is increased, anticoagulation with citrate is recommended (grade D−). CRRT without anticoagulation can be considered when coagulopathy is present (grade D−). If clotting tendency is increased predilution or the addition of prostaglandins to heparin may be helpful (grade C−).
Conclusion
Anticoagulation for CRRT must be tailored to patient characteristics and local facilities. The implementation of regional anticoagulation with citrate is worthwhile to reduce bleeding risk. Future trials should be randomized and should have sufficient power and well defined endpoints to compensate for the complexity of critical illness-related pro- and anticoagulant forces. An international consensus to define clinical endpoints is advocated.
Similar content being viewed by others
References
Van de Wetering J, Westendorp RGJ, Van der Hoeven JG, Stolk B, Feuth JDM, Chang PC (1996) Heparin use in continuous renal replacement procedure: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol 7:145–150
Davenport A (1997) The coagulation system in the critically ill patient with acute renal failure and the effect of an extracorporeal circuit. Am J Kidney Dis 30:20–27
Stefanidis I, Frank D, Maurin N (1998) Hemostasis activation markers in acute renal failure. Ren Fail 20:147–155
Cardigan RA, McGloin H, Mackie IJ, Machin SJ, Singer M (1999) Activation of the tissue factor pathway occurs during continuous venovenous hemofiltration. Kidney Int 55:1568–1574
Colucci M, Balconi G, Lorenzet R, Pietra A, Locati D, Donati MB, Semeraro N (1983) Cultured human endothelial cells generate tissue factor in response to endotoxin. J Clin Invest 71:1893–1896
Kappelmayer J, Bernabei A, Edmunds LH Jr, Edgington TS, Colman RW (1993) Tissue factor is expressed on monocytes during simulated extracorporeal circulation. Circ Res 72:1075–1081
Bastien O, French P, Paulus S, Filley S, Berruyer M, Dechavanne M, Estanove S (1995) Antithrombin III deficiency during continuous venovenous hemodialysis. Contrib Nephrol 116:154–158
Salmon J, Cardigan R, Mackie I, Cohen SL, Machin S, Singer M (1997) Continuous venovenous haemofiltration using polyacrylonitrile filters does not activate contact system and intrinsic coagulation pathways. Intensive Care Med 23:38–43
Joannes-Boyau O, Lafargue M, Honore PM, Gaucher B, Fleureau C, Janvier G (2005) Short filter lifespan during hemofiltration in sepsis: antithrombine (AT) supplementation should be a good way to sort out this problem (abstract). Blood Purif 23:169
Boldt J, Menges T, Wollbruck M, Sonneborn S, Hempelmann G (1994) Continuous hemofiltration and platelet function in critically ill patients. Crit Care Med 22:1155–6011
Holt AW, Bierer P, Bersten AD, Bury LK, Vedig AE (1996) Continuous renal replacement therapy in critically ill patients: monitoring circuit function. Anaesth Intensive Care 24:423–429
Martin PY, Chevrolet JC, Suter P, Favre H (1994) Anticoagulation in patients treated by continuous venovenous hemofiltration: a retrospective study. Am J Kidney Dis 24:806–812
Pont AC de, Oudemans-van Straaten HM, Roozendaal KJ, Zandstra DF (2000) Nadroparin versus dalteparin anticoagulation in high-volume, continuous venovenous hemofiltration: a double-blind, randomized, crossover study. Crit Care Med 28:421–425
Cutts MW, Thomas AN, Kishen R (2000) Transfusion requirements during continuous veno-venous haemofiltration: the importance of filter life. Intensive Care Med 26:1694–1697
Uchino S, Fealy N, Baldwin I, Morimatsu H, Bellomo R (2003) Pre-dilution vs. post-dilution during continuous veno-venous hemofiltration: impact on filter life and azotemic control. Nephron Clin Pract 94:94–98
Morabito S, Guzzo I, Solazzo A, Muzi L, Luciani R, Pierucci A (2003) Continuous renal replacement therapies: anticoagulation in the critically ill at high risk of bleeding. J Nephrol 16:566–571
Stefanidis I, Hagel J, Frank D, Maurin N (1996) Hemostatic alterations during continuous venovenous hemofiltration in acute renal failure. Clin Nephrol 46:199–205
Ramesh Prasad GV, Palevsky PM, Burr R, Lesko JM, Gupta B, Greenberg A (2000) Factors affecting system clotting in continuous renal replacement therapy: results of a randomized, controlled trial. Clin Nephrol 53:55–60
Baldwin I, Bellomo R, Koch B (2004) Blood flow reductions during continuous renal replacement therapy and circuit life. Intensive Care Med 30:2074–2079
Webb AR, Mythen MG, Jacobson D, Mackie IJ (1995) Maintaining blood flow in the extracorporeal circuit: haemostasis and anticoagulation. Intensive Care Med 21:84–93
Favre H, Martin Y, Spoermann C (1996) Anticoagulation in continuous extracorporeal renal replacement therapy. Semin Dialysis 9:112–118
Schetz M (2001) Anticoagulation in continuous renal replacement therapy. Contrib Nephrol 132:283–303
Davenport A, Mehta S (2002) The Acute Dialysis Quality Initiative. VI. Access and anticoagulation in CRRT. Adv Ren Replace Ther 9:273–281
Dellinger RP, Carlet JM, Masur H, Gerlach H (2004) Introduction to the Surviving Sepsis Campaign Guidelines. Crit Care Med 32:446–447
Mehta RL (1996) Anticoagulation strategies for continuous renal replacement therapies: what works? Am J Kidney Dis 28:8–14
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G (2000) Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 356:26–30
Bouman CS, Oudemans-Van Straaten HM, Tijssen JG, Zandstra DF, Kesecioglu J (2002) Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med 30:2205–2211
Hoppensteadt DA, Walenga JM, Fasanella A, Jeske W, Fareed J (1995) TFPI antigen levels in normal human volunteers after intravenous and subcutaneous administration of unfractionated heparin and a low molecular weight heparin. Thromb Res 77:175–185
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, Granger C, Ohman EM, Dalen JE (2001) Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest 119:64-94
Greaves M (2002) Control of Anticoagulation Subcommittee of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis. Limitations of the laboratory monitoring of heparin therapy. Scientific and Standardization Committee Communications: on behalf of the Control of Anticoagulation Subcommittee of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis. Thromb Haemost 87:163–164
Baker BA, Adelman MD, Smith PA, Osborn JC (1997) Inability of the activated partial thromboplastin time to predict heparin levels. Time to reassess guidelines for heparin assays. Arch Intern Med 157:2475–2479
De Waele JJ, Van Cauwenberghe S, Hoste E, Benoit D, Colardyn F (2003) The use of the activated clotting time for monitoring heparin therapy in critically ill patients. Intensive Care Med 29:325–328
Bellomo R, Teede H, Boyce N (1993) Anticoagulant regimens in acute continuous hemodiafiltration: a comparative study. Intensive Care Med 19:329–332
Leslie GD, Jacobs IG, Clarke GM (1996) Proximally delivered dilute heparin does not improve circuit life in continuous venovenous haemodiafiltration. Intensive Care Med 22:1261–1264
Tan HK, Baldwin I, Bellomo (2000) Continuous veno-venous hemofiltration without anticoagulation in high-risk patients. Intensive Care Med 26:1652–1657
Stefanidis I, Hagel J, Maurin N (1995) Influence of coagulation parameters on filter running time during continuous venovenous hemofiltration. Contrib Nephrol 116:145–149
Frydman A (1996) Low-molecular-weight heparins: an overview of their pharmacodynamics, pharmacokinetics and metabolism in humans. Haemostasis 26 [Suppl 2]:24–38
Singer M, McNally T, Screaton G, Mackie I, Machin S, Cohen SL (1994) Heparin clearance during continuous veno-venous haemofiltration. Intensive Care Med 20:212–215
Reeves JH, Cumming AR, Gallagher L, O'Brien JL, Santamaria JD (1999) A controlled trial of low-molecular-weight heparin (dalteparin) versus unfractionated heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med 27:2224–2228
Joannidis M, Kountchew J, Grote A, Bellmann R, Mayr A, Wiedermann C (2004) Unfractionated versus low-molecular-weight heparin (enoxaparin) for anticoagulation in CVVH (abstract). Intensive Care Med 30:S155
Journois D, Safran D, Castelain MH, Chanu D, Drevillon C, Barrier G (1990) Comparison of the antithrombotic effects of heparin, enoxaparin and prostacycline in continuous hemofiltration. Ann Fr Anesth Reanim 9:331–337
Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI, Zandstra DF (1999) Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 25:814–821
Reeves JH, Graan M (2003) Randomised controlled trial enoxaparin versus heparin in continuous renal replacement therapy (abstract). Blood Purif 21:207
Van Doorn KJ, Hubloue I, Verbeelen D (2004) Urea exchange efficacy during unfractionated heparin anticoagulation versus low molecular weight heparin (dalteparin) anticoagulation in continuous venovenous hemofiltration (abstract). Blood Purif 22:243–244
Knight DW, Selwyn D, Girling K (2003) Low-molecular-weight heparin for anticoagulation during continuous venovenous hemofiltration. Arch Intern Med 163:981
Farooq V, Hegarty J, Chandrasekar T, Lamerton EH, Mitra S, Houghton JB, Kalra PA, Waldek S, O'Donoghue DJ, Wood GN (2004) Serious adverse incidents with the usage of low molecular weight heparins in patients with chronic kidney disease. Am J Kidney Dis 43:531–537
Nagge J, Crowther M, Hirsh J (2002) Is impaired renal function a contraindication to the use of low-molecular-weight heparin? Arch Intern Med 162:2605–2609
Meuleman DG, Hobbelen PMJ, van Dedem G, Moelker HCT (1982) A novel anti-thrombotic heparinoid (Org 10172) devoid of bleeding inducing capacity: a survey of its pharmacological properties in experimental animal models. Thromb Res 27:353–363
Magnani HN (1993) Heparin-induced thrombocytopenia (HIT): an overview of 230 patients treated with Orgaran (Org 10172). Thromb Haemost 70:554–561
Polkinghorne KR, McMahon LP, Becker GJ (2002) Pharmacokinetic studies of dalteparin (Fragmin), enoxaparin (Clexane), and danaparoid sodium (Orgaran) in stable chronic hemodialysis patients. Am J Kidney Dis 40:990–995
Lindhoff-Last E, Betz C, Bauersachs R (2001) Use of a low-molecular-weight heparinoid (danaparoid sodium) for continuous renal replacement therapy in intensive care patients. Clin Appl Thromb Hemost 7:300–304
Wester JPJ (2004) Guidelines for anticoagulation with danaparoid sodium and lepirudin in continuous venovenous hemofiltration. Neth J Crit Care 8:293–301
Warkentin TE, Greinacher A (2005) Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126:311–337
Warkentin TE, Cook RJ, Marder VJ, Sheppard JA, Moore JC, Eriksson BI, Greinacher A, Kelton JG (2005) Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood 106:3791–3796
Martel N, Lee J, Wells PS (2005) Risk of heparin induced thrombocytopenia with unfractionated and low molecular weight heparin thromboprophylaxis: a meta-analysis. Blood 106:2710–2715
Wester JPJ, Haas FJ, Biesma DH, Leusink JA, Veth G (2004) Thrombosis and hemorrhage in heparin-induced thrombocytopenia in seriously ill patients. Intensive Care Med 30:1927–1934
Koopman MM, Buller HR (2003) Short- and long-acting synthetic pentasaccharides. J Intern Med 254:335–342
Savi P, Chong BH, Greinacher A, Gruel Y, Kelton JG, Warkentin TE, Eichler P, Meuleman D, Petitou M, Herault JP, Cariou R, Herbert JM (2005) Effect of fondaparinux on platelet activation in the presence of heparin-dependent antibodies: a blinded comparative multicenter study with unfractionated heparin. Blood 105:139–144
Bijsterveld NR, Moons AH, Boekholdt SM, van Aken BE, Fennema H, Peters RJ, Meijers JC, Buller HR, Levi M (2002) Ability of recombinant factor VIIa to reverse the anticoagulant effect of the pentasaccharide fondaparinux in healthy volunteers. Circulation 106:2550–2554
Greinacher A (2004) Lepirudin for the treatment of heparin-induced thrombocytopenia. In: Warkentin TE, Greinacher A (ed) Heparin-induced thrombocytopenia, 3rd edn. Dekker, New York, pp 397–436
Greinacher A, Eichler P, Lubenow N, Kwasny H, Luz M (2000) Heparin-induced thrombocytopenia with thromboembolic complications: meta-analysis of 2 prospective trials to assess the value of parenteral treatment with lepirudin and its therapeutic aPTT range. Blood 96:846–881
Fischer KG, van de Loo A, Bohler J (1999) Recombinant hirudin (lepirudin) as anticoagulant in intensive care patients treated with continuous hemodialysis. Kidney Int Suppl 72:46–50
Kern H, Ziemer S, Kox WJ (1999) Bleeding after intermittent or continuous r-hirudin during CVVH. Intensive Care Med 25:1311–1314
Muhl E, Siemens HJ, Kujath P, Bruch HP (2002) Therapy and monitoring of heparin-induced thrombocytopenia type II in critically ill patients during continuous venovenous hemodiafiltration: comparison of aPTT and ecarin clotting tome for monitoring of r-hirudin therapy. J Intensive Care 17:34–40
Wester JPJ, ten Cate J, Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI, Zandstra DF (2003) Lepirudin anticoagulation in critically ill patients with (suspected) heparin-induced thrombocytopenia and thrombosis. J Thromb Haemost 1 [Suppl 1]:P1907
Fischer KG (2002) Hirudin in renal insufficiency. Semin Thromb Hemost 28:467–482
Eichler P, Friesen HJ, Lubenow N, Jaeger B, Greinacher A (2000) Antihirudin antibodies in patients with heparin-induced thrombocytopenia treated with lepirudin: incidence, effects on aPTT, and clinical relevance. Blood 96:2373–2378
Greinacher A, Lubenow N, Eichler P (2003) Anaphylactic and anaphylactoid reactions associated with lepirudin in patients with heparin-induced thrombocytopenia. Circulation 108:2062–2065
Vargas Hein O, von Heymann C, Lipps M, Ziemer S, Ronco C, Neumayer HH, Morgera S, Welte M, Kox WJ, Spies C (2001) Hirudin versus heparin for anticoagulation in continuous renal replacement therapy. Intensive Care Med 27:673–679
Vargas Hein O, von Heymann C, Diehl T, Ziemer S, Ronco C, Morgera S, Siebert G, Kox WJ, Neumayer HH, Spies C (2004) Intermittent hirudin versus continuous heparin for anticoagulation in continuous renal replacement therapy. Ren Fail 26:297–303
Murray PT, Reddy BV, Grossman EJ, Hammes MS, Trevino S, Ferrell J, Tang I, Hursting MJ, Shamp TR, Swan SK (2004) A prospective comparison of three argatroban treatment regimens during hemodialysis in end-stage renal disease. Kidney Int 66:2446–2453
Tang IY, Cox DS, Patel K, Reddy BV, Nahlik L, Trevino S, Murray PT (2005) Argatroban and renal replacement therapy in patients with heparin-induced thrombocytopenia. Ann Pharmacother 39:231–236
Boccardo P, Melacini D, Rota S, Mecca G, Boletta A, Casiraghi F, Gianese F (1997) Individualized anticoagulation with dermatan sulphate for haemodialysis in chronic renal failure. Nephrol Dial Transplant 12:2349–2354
Gianese F, Nurmohamed MT, Imbimbo BP, Buller HR, Berckmans RJ, Ten Cate JW (1993) The pharmacokinetics and pharmacodynamics of dermatan sulphate MF701 during haemodialysis for chronic renal failure. Br J Clin Pharmacol 35:335–339
Bermond F, Fenocchio CM, Cantaluppi V, Guarena C, Pacitti A (2005) Anticoagulation with dermatan sulphate for renal replacement therapy in intensive care units (abstract). Blood Purif 23:167
Langenecker SA, Felfernig M, Werba A, Mueller CM, Chiari A, Zimpfer M (1994) Anticoagulation with prostacyclin and heparin during continuous venovenous hemofiltration. Crit Care Med 22:1774–1781
Kozek-Langenecker SA, Kettner SC, Oismueller C, Gonano C, Speiser W, Zimpfer M (1998) Anticoagulation with prostaglandin E1 and unfractionated heparin during continuous venovenous hemofiltration. Crit Care Med 26:1208–1212
Kozek-Langenecker SA, Spiss CK, Gamsjager T, Domenig C, Zimpfer M (2002) Anticoagulation with prostaglandins and unfractionated heparin during continuous venovenous haemofiltration: a randomized controlled trial. Wien Klin Wochenschr 114:96–101
Fiaccadori E, Maggiore U, Rotelli C, Minari M, Melfa L, Cappe G, Cabassi A (2002) Continuous haemofiltration in acute renal failure with prostacyclin as the sole anti-haemostatic agent. Intensive Care Med 28:586–593
Davenport A, Will EJ, Davinson AM (1994) Comparison of the use of standard heparin and prostacyclin anticoagulation in spontaneous and pump-driven extracorporeal circuits in patients with combined acute renal and hepatic failure. Nephron 66:431–437
Kozek-Langenecker SA, Spiss CK, Michalek-Sauberer A, Felfernig M, Zimpfer M (2003) Effect of prostacyclin on platelets, polymorphonuclear cells, and heterotypic cell aggregation during hemofiltration. Crit Care Med 31:864–868
Bihari DJ, Tinker J (1988) The therapeutic value of vasodilator prostaglandins in multiple organ failure associated with sepsis. Intensive Care Med 15:2–7
Uchiba M, Okajima K, Murakami K, Okabe H, Takatsuki K (1995) Inhibition of tissue factor-factor VIIa by nafamostat mesilate; a reply to the rebuttal. Thromb Res 77:381–382
Nakae H, Tajimi K (2003) Pharmacokinetics of nafamostat mesilate during continuous hemodiafiltration with a polyacrylonitrile membrane. Ther Apher Dial 7:483–485
Ohtake Y, Hirasawa H, Sugai T, Oda S, Shiga H, Matsuda K, Kitamura N (1991) Nafamostat mesylate as anticoagulant in continuous hemofiltration and continuous hemodiafiltration. Contrib Nephrol 93:215–217
Hu ZJ, Iwama H, Suzuki R, Kobayashi S, Akutsu I (1999) Time course of activated coagulation time at various sites during continuous haemodiafiltration using nafamostat mesilate. Intensive Care Med 25:524–527
Okada H, Suzuki H, Deguchi N, Saruta T (1992) Agranulocytosis in a haemodialysed patient induced by a proteinase inhibitor, nafamostate mesilate. Nephrol Dial Transplant 7:980
Ookawara S, Tabei K, Sakurai T, Sakairi Y, Furuya H, Asano Y (1996) Additional mechanisms of nafamostat mesilate-associated hyperkalaemia. Eur J Clin Pharmacol 51:149–145
Higuchi N, Yamazaki H, Kikuchi H, Gejyo F (2000) Anaphylactoid reaction induced by a protease inhibitor, nafamostat mesilate, following nine administrations in a hemodialysis patient. Nephron 86:400–401
Esmon CT (2003) The protein C pathway. Chest 124:26–32
Pont AC de, Bouman CS, de Jonge E, Vroom MB, Buller HR, Levi M (2003) Treatment with recombinant human activated protein C obviates additional anticoagulation during continuous venovenous hemofiltration in patients with severe sepsis. Intensive Care Med 29:1205
Mehta RL, McDonald BR, Aguilar MM, Ward DM (1990) Regional citrate anticoagulation for continuous arteriovenous hemodialysis in critically ill patients. Kidney Int 38:976–981
Fiore G, Donadio PP, Gianferrari P, Santacroce C, Guermani A (1998) CVVH in postoperative care of liver transplantation. Minerva Anestesiol 64:83–87
Uchino S, Fealy N, Baldwin I, Morimatsu H, Bellomo R (2004) Continuous venovenous hemofiltration without anticoagulation. ASAIO J 50:76–80
Naka T, Wan L, Bellomo R, Wang BZ, Jones R, Berry R, Angus P, Gow P (2004) Kidney failure associated with liver transplantation or liver failure: the impact of continuous veno-venous hemofiltration. Int J Artif Organs 27:949–955
Apsner R, Schwarzenhofer M, Derfler K, Zauner C, Ratheiser K, Kranz A (1997) Impairment of citrate metabolism in acute hepatic failure. Wien Klin Wochenschr 109:123–127
Kramer L, Bauer E, Joukhadar C, Strobl W, Gendo A, Madl C, Gangl A (2003) Citrate pharmacokinetics and metabolism in cirrhotic and noncirrhotic critically ill patients. Crit Care Med 31:2450–2455
Mehta RL, McDonald BR, Ward DM (1991) Regional citrate anticoagulation for continuous arteriovenous hemodialysis. An update after 12 months. Contrib Nephrol 93:210–214
Ward DM, Mehta RL (1993) Extracorporeal management of acute renal failure patients at high risk of bleeding. Kidney Int 43:237–244
Aspner R, Druml W (1998) More on anticoagulation for continuous hemofiltration. N Engl J Med 338:131–132
Thoenen M, Schmid ER, Binswanger U, Schuepbach R, Aerne D, Schmidlin D (2002) Regional citrate anticoagulation using a citrate-based substitution solution for continuous venovenous hemofiltration in cardiac surgery patients. Wien Klin Wochenschr 114:108–114
Hofmann RM, Maloney C, Ward DM, Becker BN (2002) A novel method for regional citrate anticoagulation in continuous venovenous hemofiltration (CVVHF). Ren Fail 24:325–335
Gabutti L, Marone C, Colucci G, Duchini F, Schonholzer C (2002) Citrate anticoagulation in continuous venovenous hemodiafiltration: a metabolic challenge. Intensive Care Med 28:1419–1425
Tobe SW, Aujla P, Walele AA, Oliver MJ, Naimark DM, Perkins NJ, Beardsall M (2003) A novel regional citrate anticoagulation protocol for CRRT using only commercially available solutions. J Crit Care 18:121–129
Mitchell A, Daul AE, Beiderlinden M, Schafers RF, Heemann U, Kribben A, Peters J, Philipp T, Wenzel RR (2003) A new system for regional citrate anticoagulation in continuous venovenous hemodialysis (CVVHD). Clin Nephrol 59:106–114
Maccariello E, Valente C, Nogueira L, Serpa L, Rocha E (2003) Regional citrate anticoagulation: impact on membrane survival (abstract). Blood Purif 21:183
Swartz R, Pasko D, O'Toole J, Starmann B (2004) Improving the delivery of continuous renal replacement therapy using regional citrate anticoagulation. Clin Nephrol 61:134–143
Morgera S, Scholle C, Voss G, Haase M, Vargas Hein O, Krausch D, Melzer C, Rosseau S, Zuckermann-Becker H, Neumayer HH (2004) Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: single-center experience. Nephron Clin Pract 97:c131–c136
Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois B, Damas P (2004) Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med 30:260–265
Kutsogiannis DJ, Gibney RT, Stollery D, Gao J (2005) Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int 67:2361–2367
Bos JC, Grooteman MP, van Houte AJ, Schoorl M, van Limbeek J, Nube MJ (1997) Low polymorphonuclear cell degranulation during citrate anticoagulation: a comparison between citrate and heparin dialysis. Nephrol Dial Transplant 12:1387–1393
Hofbauer R, Moser D, Frass M, Oberbauer R, Kaye AD, Wagner O, Kapiotis S, Druml W (1999) Effect of anticoagulation on blood membrane interactions during hemodialysis. Kidney Int 56:1578–1583
Carr JA, Silverman N (1999) The heparin-protamine interaction. A review. J Cardiovasc Surg 40:659–666
Rossmann P, Matoušovic K, Horáèek V (1982) Protamine-heparin aggregates. Virchows Arch 40:81–98
Biancofiore G, Esposito M, Bindi L, Stefanini A, Bisa M, Boldrini A, Consani G, Filipponi F, Mosca F (2003) Regional filter heparinization for continuous veno-venous hemofiltration in liver transplant recipients. Minerva Anestesiol 69:527–538
Van der Voort PH, Gerritsen RT, Kuiper MA, Egbers PH, Kingma WP, Boerma EC (2005) Filter run time in CVVH: pre- versus post-dilution and nadroparin versus regional heparin-protamine anticoagulation. Blood Purif 23:175–180
Kaplan AA (1985) Predilution versus postdilution for continuous arteriovenous hemofiltration. Trans Am Soc Artif Intern Organs 31:28–32
Honore PM, Wittebolle X, Lozano A (1997) Evaluation of the predilution technique in reducing the occurence of bleeding during CRRT in critically ill patients. Efficacy of predilution in reducing the amount of anticoagulation during CVVH (abstract). Crit Care [Suppl 1]:P97
Clark WR, Turk JE, Kraus MA, Gao D (2003) Dose determinants in continuous renal replacement therapy. Artif Organs 27:815–820
Kumar VA, Craig M, Depner TA, Yeun JY (2000) Extended daily dialysis: a new approach to renal replacement for acute renal failure in the intensive care unit. Am J Kidney Dis 36:294–300
Kielstein JT, Kretschmer U, Ernst T, Hafer C, Bahr MJ, Haller H, Fliser D (2004) Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis 43:342–349
Opatrny K Jr, Polanska K, Krouzecky A, Vit L, Novak I, Kasal E (2002) The effect of heparin rinse on the biocompatibility of continuous veno-venous hemodiafiltration. Int J Artif Organs 25:520–528
Reeves JH, Seal PF, Voss AL, O'Connor C (1997) Albumin priming does not prolong hemofilter life. ASAIO J 43:193–196
Baldwin I, Tan HK, Bridge N, Bellomo R (2002) Possible strategies to prolong circuit life during hemofiltration: three controlled studies. Ren Fail 24:839–848
Sieffert E, Mateo J, Deligeon N, Payen D (1997) Continuous veno-venous hemofiltration (CVVH) using heparin-coated or non heparin-coated membranes in critically ill patients (abstract). Blood Purif 15:125
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Oudemans-van Straaten, H.M., Wester, J.P.J., de Pont, A.C.J.M. et al. Anticoagulation strategies in continuous renal replacement therapy: can the choice be evidence based?. Intensive Care Med 32, 188–202 (2006). https://doi.org/10.1007/s00134-005-0044-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0044-y