Abstract
Background
The study investigates whether adolescents referred to specialty mental health services from local services differ from adolescents who only have received help for psychiatric problems locally. If so, which factors associate strongest with referral?
Method
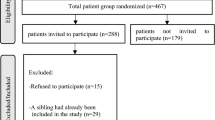
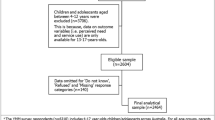
Adolescents (n = 76) from an adolescent population sample (N = 2,538) who had received help during the last year for mental problems from local services were compared to a clinical sample of adolescents (N = 129) referred to specialty mental health services from such local services. Comparisons were made according to scores on the Youth Self-Report (YSR); depressive symptoms; family functioning; attachment to parents; self-concept; coping styles; response styles; dysfunctional attitudes; negative life events; daily hassles; socio-demographics.
Results
As compared to adolescents receiving help locally, adolescents in specialty mental health care scored higher on YSR internalising syndrome; YSR attention problems; YSR thought problems; suicidality; psychosocial stressors; knowing someone who had attempted suicide; parental divorce; substance use; recent moves; living in lodgings; lost a pal or boy/girlfriend; and lower on attachment to parents. Multivariate logistic regression analysis identified four factors associated with receiving specialty mental health care: low family functioning; moved previous year; knowing someone who had attempted suicide; own suicidality.
Conclusions
Family functioning as reported by the adolescents, and not mental health problems except for suicidality, was found to be the strongest associated with referral to specialty mental health services. Contrary to findings from many other studies, referral was associated with internalising problems, not externalising ones.
Similar content being viewed by others
References
Almqvist F, Puura K, Kumpulainen K, Tuompo-Johansson E, Henttonen I, Huikko E, Linna S, Ikaheimo K, Aronen E, Katainen S, Piha J, Moilanen I (1987) Psychiatric disorders in 8–9-year-old children based on a diagnostic interview with the parents. Eur Child Adolesc Psychiatry 1999 8(Suppl 4):17–28
Anderson JC, Williams S, McGee R, Silva PA (1987) DSM-III disorders in preadolescent children. Prevalence in a large sample from the general population. Arch Gen Psychiatry 44(1):69–76
Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, Costello EJ (2002) Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psychiatry 59(10):893–901
Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM (1996) The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 53(12):1129–1136
Fergusson DM, Horwood LJ, Lynskey MT (1993) Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. J Am Acad Child Adolesc Psychiatry 32(6):1127–1134
Kroes M, Kalff AC, Kessels AG, Steyaert J, Feron FJ, van Someren AJ, Hurks PP, Hendriksen JG, van Zeben TM, Rozendaal N, Crolla IF, Troost J, Jolles J, Vles JS (2001) Child psychiatric diagnoses in a population of Dutch schoolchildren aged 6 to 8 years. J Am Acad Child Adolesc Psychiatry 40(12):1401–1409
Lavik NJ (1976) Ungdoms mentale helse. Universitetsforlaget, Oslo
McGee R, Feehan M, Williams S, Partridge F, Silva PA, Kelly J (1990) DSM-III disorders in a large sample of adolescents. J Am Acad Child Adolesc Psychiatry 29(4):611–619
Offord DR, Boyle MH, Fleming JE, Blum HM, Grant NI (1989) Ontario Child Health Study. Summary of selected results. Can J Psychiatry 34(6):483–491
Verhulst FC, Berden GF, Sanders-Woudstra JA (1985) Mental health in Dutch children: (II). The prevalence of psychiatric disorder and relationship between measures. Acta Psychiatr Scand Suppl 324:1–45
Verhulst FC, van der Ende J (1997) Factors associated with child mental health service use in the community. J Am Acad Child Adolesc Psychiatry 36(7):901–909
Costello EJ (1989) Child psychiatric disorders and their correlates: a primary care pediatric sample. J Am Acad Child Adolesc Psychiatry 28(6):851–855
Zwaanswijk M, Van der Ende J, Verhaak PF, Bensing JM, Verhulst FC (2003) Factors associated with adolescent mental health service need and utilization. J Am Acad Child Adolesc Psychiatry 42(6):692–700
Achenbach TM (1991) Manual for the child behavior checklist/4–18 and 1991 profile. University of Vermont: Department of Psychiatry, Burlington
Sourander A, Helstela L, Ristkari T, Ikaheimo K, Helenius H, Piha J (2001) Child and adolescent mental health service use in Finland. Soc Psychiatry Psychiatr Epidemiol 36(6):294–298
Costello EJ, Janiszewski S (1990) Who gets treated? Factors associated with referral in children with psychiatric disorders. Acta Psychiatr Scand 81(6):523–529
Angold A, Messer SC, Stangl D, Farmer EM, Costello EJ, Burns BJ (1998) Perceived parental burden and service use for child and adolescent psychiatric disorders. Am J Public Health 88(1):75–80
Cohen P, Kasen S, Brook JS, Struening EL (1991) Diagnostic ors of treatment patterns in a cohort of adolescents. J Am Acad Child Adolesc Psychiatry 30(6):989–993
Wu P, Hoven CW, Bird HR et al (1999) Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry 38(9):1081–1090, discussion 1090–1092
Romano E, Tremblay RE, Vitaro F, Zoccolillo M, Pagani L (2001) Prevalence of psychiatric diagnoses and the role of perceived impairment: findings from an adolescent community sample. J Child Psychol Psychiatry 42(4):451–461
Mesman J, Koot HM (2000) Child-reported depression and anxiety in preadolescence: I. Associations with parent- and teacher-reported problems. J Am Acad Child Adolesc Psychiatry 39(11):1371–1378
Cohen P, Hesselbart CS (1993) Demographic factors in the use of children’s mental health services. Am J Public Health 83(1):49–52
Zahner GE, Daskalakis C (1997) Factors associated with mental health, general health, and school-based service use for child psychopathology. Am J Public Health 87(9):1440–1448
Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, Regier D (1997) Representativeness of clinical samples of youths with mental disorders: a preliminary population-based study. J Abnorm Psychol 106(1):3–14
Garralda ME, Bailey D (1988) Child and family factors associated with referral to child psychiatrists. Br J Psychiatry 153:81–89
John LH, Offord DR, Boyle MH, Racine YA (1995) Factors in use of mental health and social services by children 6–16 years old: findings from the Ontario Child Health Study. Am J Orthopsychiatry 65(1):76–86
Sund AM, Larsson B, Wichstrom L (2001) Depressive symptoms among young Norwegian adolescents as measured by the Mood and Feelings Questionnaire (MFQ). Eur J Child Adolesc Psychiatry 10:222–229
Edelbrock C, Costello AJ (1988) Convergence between statistically derived behavior problem syndromes and child psychiatric diagnoses. J Abnorm Child Psychol 16(2):219–231
Fisher PW, Shaffer D, Piacentini JC, Lapkin J, Kafantaris V, Leonard H, Herzog DB (1993) Sensitivity of the Diagnostic Interview Schedule for Children, 2nd edition (DISC-2.1) for specific diagnoses of children and adolescents. J Am Acad Child Adolesc Psychiatry 32(3):666–673
Kasius MC, Ferdinand RF, van den Berg H, Verhulst FC (1997) Associations between different diagnostic approaches for child and adolescent psychopathology. J Child Psychol Psychiatry 38(6):625–632
Kazdin AE, Heidish IE (1984) Convergence of clinically derived diagnoses and parent checklists among inpatient children. J Abnorm Child Psychol 12(3):421–435
Morgan CJ, Cauce AM (1999) ing DSM-III-R disorders from the youth self-report: analysis of data from a field study. J Am Acad Child Adolesc Psychiatry 38(10):1237–1245
Weinstein SR, Noam GG, Grimes K, Stone K, Schwab-Stone M (1990) Convergence of DSM-III diagnoses and self-reported symptoms in child and adolescent inpatients. J Am Acad Child Adolesc Psychiatry 29(4):627–634
Angold A (1989) Structured assessment of psychopathology in children and adolescents. In: Thompson C (ed) The instruments of psychiatric research. John Wiley, Chichester, pp271–304
Goodyer IM, Herbert J, Tamplin A, Secher SM (1997) Pearson J. Short-term outcome of major depression: II. Life events, family dysfunction, and friendship difficulties as ors of persistent disorder. J Am Acad Child Adolesc Psychiatry 36(4):474–480
Pellegrino JF, Singh NN, Carmanico SJ (1999) Concordance among three diagnostic procedures for identifying depression in children and adolescents. J Emotional Behav Disord 7:118–127
Wood A, Kroll L, Moore A, Harrington R (1995) Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. J Child Psychol Psychiatry 36(2):327–334
Byles J, Byrne C, Boyle MH, Offord DR (1988) Ontario Child Health Study: reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process 27(1):97–104
Armsden GC, Greenberg MT (1987) The inventory of parent and peer attachment: individual differences and their relationships to psychological well-being in adolescence. J Youth Adolesc 16:427–454
Weissman AN, Beck AT (1978) Development and validation of the Dysfunctional Attitude Scale
Andrews JA, Lewinsohn PM, Hops H, Roberts RE (1993) Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychol Rep 73:1019–1046
Endler NS, Parker JDA (1990) Multidimensional assessment of coping: a critical evaluation. J Personality Soc Psychol 58:844–854
Nolen-Hoeksema S (2000) The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 109(3):504–511
Fenigstein A, Scheier MF, Buss AH (1975) Public and private self-consciousness assessment and theory. J Consult Clin Psychol 43:522–527
Sund AM, Larsson B, Wichstrom L (2003) Psychosocial correlates of depressive symptoms among 12–14-year-old Norwegian adolescents. J Child Psychol Psychiatry 44(4):588–597
Wichstrom L (1995) Social, psychological and physical correlates of eating problems. A study of the general adolescent population in Norway. Psychol Med 25(3):567–579
Anderson HW, Halsteinli V (2000) Hvordan kan mål om 5 prosent nås? (How can the goal of 5 percent be met?). Hagen H. Psykiatritjenesten 1999 – omstilling og vekst (Psychiatric Services 1999 – Restructuring and Growth). Unimed NIS, SAMDATA/Kommuneforbundet, Trondheim, Norway, pp 85–94
Reigstad B, Jørgensen K, Wichstrøm L (2004) Changes in referrals to child and adolescents psychiatric services in Norway 1992–2001. Soc Psychiatry Psychiatr Epidemiol 39(10): 818–827
Sayal K (2004) The role of parental burden in child mental health service use: longitudinal study. J Am Acad Child Adolesc Psychiatry 43:1328–1333
Farmer EMZ, Burns BJ, Philips SD, Angold A, Costello EJ (2003) Pathways into and through mental health services for children and adolescence. Psychiatr Serv 54:60–66
Logan DE, King CA (2002) Parental identification of depression and mental health service use among depressed adolescents. J Am Acad Child Adolesc Psychiatry 41:296–304
Palosaari U, Aro H, Laippala P (1996) Parental divorce and depression in young adulthood: adolescents’ closeness to parents and self-esteem as mediating factor. Acta Psychiatr Scand 93(1):20–26
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey 51:8–19
Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY (2004) Stressors and child and adolescent psychopathology: measurement issues and prospective effect. J Clin Child Adolesc Psychol 33:412–425
Fergusson DM, Horwood LJ, Swain-Campbell N (2002) Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction 97:1123–1135
Poulin C, Hand D, Boudreau B, Santor D (2005) Gender differences in the association between substance use and elevated depressive symptoms in a general adolescent population. Addiction 100:525–535
Steuber TL, Danner F (2006) Adolescent smoking and depression: which comes first? Addict Behav 44(1):69–76
Wichstrom L (2000) ors of adolescent suicide attempts: a nationally representative longitudinal study of Norwegian adolescents. J Am Acad Child Adolesc Psychiatry 39(5):603–610
Just N, Alloy LB (1997) The response styles theory of depression: tests and an extension of the theory. J Abnorm Psychol 106(2):221–229
Nolen-Hoeksema S (1991) Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol 100(4):569–582
McWilliams LA, Cox BJ, Enns MW (2003) Use of coping inventory for stressful situations in a clinically depressed sample: factor structure, personality correlates, and prediction of distress. J Clin Psychol 59:423–437
Acknowledgement
This study was funded with a grant from the Norwegian Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reigstad, B., Jørgensen, K., Sund, A.M. et al. Adolescents referred to specialty mental health care from local services and adolescents who remain in local treatment: what differs?. Soc Psychiat Epidemiol 41, 323–331 (2006). https://doi.org/10.1007/s00127-005-0027-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0027-x