Abstract
Aims/hypothesis
We aimed to examine the association between type 2 diabetes and major subtypes of heart disease, to assess the role of genetic and early-life familial environmental factors in this association and to explore whether and to what extent a healthy lifestyle mitigates the risk of heart disease related to type 2 diabetes.
Methods
In this prospective nested case–control study based on the Swedish Twin Registry, 41,463 twin individuals who were aged ≥40 and heart disease-free were followed up for 16 years (from 1998 to 2014) to detect incident heart disease. Type 2 diabetes was ascertained from self-report, the National Patient Registry and glucose-lowering medication use. Heart disease diagnosis (including coronary heart disease, cardiac arrhythmias and heart failure) and onset age were identified from the National Patient Registry. Healthy lifestyle-related factors consisted of being a non-smoker, no/mild alcohol consumption, regular physical activity and being non-overweight. Participants were divided into three groups according to the number of lifestyle-related factors: (1) unfavourable (participants who had no or only one healthy lifestyle factor); (2) intermediate (any two or three); and (3) favourable (four). Generalised estimating equation models for unmatched case–control design and conditional logistic regression for co-twin control design were used in data analyses.
Results
Of all participants, 2304 (5.5%) had type 2 diabetes at baseline. During the observation period, 9262 (22.3%) had any incident heart disease. In unmatched case–control analyses and co-twin control analyses, the multi-adjusted OR and 95% CI of heart disease related to type 2 diabetes was 4.36 (3.95, 4.81) and 4.89 (3.88, 6.16), respectively. The difference in ORs from unmatched case–control analyses vs co-twin control analyses was statistically significant (OR 1.57; 95% CI 1.42, 1.73; p < 0.001). In stratified analyses by type 2 diabetes, compared with an unfavourable lifestyle, an intermediate lifestyle or a favourable lifestyle was associated with a significant 32% (OR 0.68; 95% CI 0.49, 0.93) or 56% (OR 0.44; 95% CI 0.30, 0.63) decrease in heart disease risk among patients with type 2 diabetes, respectively. There were significant additive and multiplicative interactions between lifestyle and type 2 diabetes on heart disease.
Conclusions/interpretation
Type 2 diabetes is associated with more than fourfold increased risk of heart disease. The association still remains statistically significant, even after fully controlling for genetic and early-life familial environmental factors. However, greater adherence to a healthy lifestyle may significantly mitigate the risk of heart disease related to type 2 diabetes.

Graphical abstract
Similar content being viewed by others

Introduction
Worldwide, diabetes affected 451 million people (8.4% of the world’s population) in 2017, and this number might dramatically rise to 693 million (9.9%) by 2045 [1]. Patients with type 2 diabetes are at increased risk of several chronic diseases and associated clinical complications, such as heart disease [2], which, in turn, is associated with cerebral vascular disease, dementia, disability and premature mortality [3].
Coronary heart disease, heart failure and cardiac arrhythmias are the common types of heart disease [3]. Thus far, population-based longitudinal studies have consistently shown that type 2 diabetes is associated with the risk of total CVD, mainly including coronary heart disease and stroke [2, 4,5,6,7]. However, the associations between type 2 diabetes and certain subtypes of heart disease independently remain unclear. Several cohort studies examined the relationship between type 2 diabetes and atrial fibrillation and flutter, and showed inconsistent results [8,9,10,11,12]. Discrepancies in previous findings can be attributed to the different study populations, follow-up times and sample size, and lack of consideration of possible confounders.
Although type 2 diabetes may be linked to heart disease through several biologically plausible pathways, our understanding of the mechanisms for such an association is still limited. Both type 2 diabetes and heart disease are complex genetic and lifestyle-related disorders [3]. Genetic and early-life familial environmental factors may contribute to the development of type 2 diabetes [13] and heart disease [14]. However, their role in the association between type 2 diabetes and heart disease is uncertain. Twins are generally reared together and share genetic background. Thus, twin studies provide the possibility to assess whether genetic and/or early familial environmental factors play a role in a given association [15]. In addition, previous studies have suggested that an individual healthy lifestyle factor (such as maintaining a normal weight, being a non-smoker, non-heavy drinking or regular exercise) was associated with lower risk of both type 2 diabetes and CVD in the general population [3, 16]. Currently, accumulating evidence has shown that adopting an overall and combined healthy lifestyle can be a more effective prevention strategy for patients with type 2 diabetes to reduce the risk of cardiovascular complications (such as cause-specific mortality rate) [17, 18]. However, the question remains whether and to what extent a combined healthy lifestyle may counteract the risk of heart disease associated with type 2 diabetes.
In the current study, we sought to: (1) examine the association between type 2 diabetes and the risk of heart disease including its major subtypes; (2) explore whether genetic and early-life familial environmental factors play a role in this association; and (3) investigate whether and to what extent a healthy lifestyle could mitigate the risk of heart disease related to type 2 diabetes.
Methods
Study population
This prospective, nested case–control study included twins from the nationwide Swedish Twin Registry (STR), which was started in the 1960s [19]. In 1998–2002, all living twins in the registry who were born in 1958 or earlier were invited to participate in the Screening Across the Lifespan Twin study (SALT), a full-scale screening that gathered data on an extended set of variables via computer-assisted telephone interviews. Out of 44,919 twin individuals eligible for the telephone interview, we excluded 3184 with heart disease before screening and 272 with type 1 diabetes, resulting in 41,463 individuals with data for the current analyses (Fig. 1).
Data collection
Information on age, sex, educational attainment, marital status and zygosity was obtained from the SALT survey [19]. All twins were categorised as monozygotic, dizygotic or of undetermined zygosity. Education was defined as the maximum years of formal schooling attained, and dichotomised into <8 vs ≥8 years. Marital status was defined as married/cohabiting vs single (including divorced and widows/widowers).
Information on history of type 2 diabetes and heart disease was derived from the National Patient Registry (NPR), which covers all inpatient diagnoses in Sweden from the 1960s to the end of 2014, and outpatient (specialist clinic) diagnoses since 2001. Each medical record in the NPR included up to eight discharge diagnoses according to the ICD. The seventh revision (ICD-7) was used up to 1968, the eighth revision (ICD-8) from 1969 to 1986, the ninth revision (ICD-9) from 1987 to 1996 and the tenth revision (ICD-10) since 1997.
All participants provided informed consent. The data collection procedures were approved by the Regional Ethics Committee at Karolinska Institutet, Stockholm, Sweden, and by the Institutional Review Board of the University of Southern California, USA.
Ascertainment of type 2 diabetes
Type 2 diabetes was ascertained based on self- and informant-reported history of diabetes, glucose-lowering medication use or the NPR (ICD-7 code 260; ICD-8 and -9 code 250; and ICD-10 codes E10–E14). The age at type 2 diabetes onset was estimated according to the earliest recorded date of type 2 diabetes in the NPR or the date of type 2 diabetes onset available in SALT.
Assessment of heart disease
Information on heart disease diagnoses (ICD-7 codes 420, 433 and 434; ICD-8 and -9 codes 410–414, 427 and 428; and ICD-10 codes I20–I25 and I48–I50) was obtained from the NPR. According to the ICD codes, the major subtypes of heart disease included: (1) coronary heart disease: angina pectoris, acute myocardial infarction, chronic ischaemic heart disease and other coronary heart disease (such as coronary thrombosis and Dressler’s syndrome); (2) cardiac arrhythmias: atrial fibrillation and flutter, and other cardiac arrhythmias (such as ventricular fibrillation and flutter, atrial premature depolarisation and junctional premature depolarisation); and (3) heart failure: congestive heart failure, left ventricular failure and unspecified heart failure. The age of heart disease onset was estimated as the earliest date that a heart disease diagnosis was recorded in the NPR.
Assessment of lifestyle-related factors
Information on smoking status, alcohol consumption, physical activity and BMI was obtained from the SALT survey. Smoking status was dichotomised as never vs ever being a smoker. Data on alcohol consumption were collected by a question on drinking habits, ‘Think about your use of alcohol over your entire life. Has there ever been a period in your life when you drank too much?’, with two response options: (1) ‘no’; and (2) ‘yes’. We defined ‘no’ as ‘no/mild drinking’ and ‘yes’ as ‘heavy drinking’. Data on physical activity were collected by a question on average exercise, with seven response options: (1) ‘almost never’; (2) ‘much less than average’; (3) ‘less than average’; (4) ‘average’; (5) ‘more than average’; (6) ‘much more than average’; and (7) ‘maximum’ [20]. For the analyses, we combined these categories into two groups and defined ‘low’ as exercise ‘almost never’ to ‘much less than average’, and ‘regular’ physical activity as ‘less than average’ to ‘maximum’. BMI was calculated as weight (kg) divided by height squared (m2), and was categorised as non-overweight (BMI <25) and overweight (BMI ≥25).
In the current study, we considered four healthy lifestyle-related factors: being a non-smoker, no/mild alcohol consumption, regular physical activity and being non-overweight. Participants were divided into three groups according to the number of lifestyle-related factors: (1) unfavourable: participants who had no or only one healthy lifestyle factor; (2) intermediate: those who had any two or three healthy lifestyle factors; and (3) favourable: those who had four healthy lifestyle factors.
Statistical analysis
The characteristics of participants in different groups were compared using χ2 tests, t test and Mann–Whitney test. Generalised estimating equation (GEE) models were used to analyse the unmatched case–control data while controlling for the clustering of twins within a pair. To examine the associations between type 2 diabetes and risk of heart disease independently, we looked at the first onset of one specific subtype of heart disease with no others. Data for the co-twin control study were analysed by using conditional logistic regression, in which twin pairs were discordant for outcome; thus, cases and control participants were comparable with respect to early-life familial environmental factors (such as shared childhood socioeconomic status and adolescent environment) and genetic background (monozygotic twins shared 100% of their genetic background and dizygotic twins shared only 50%) [15]. In both GEE and conditional logistic regression, the ORs and 95% CIs were estimated for the association between type 2 diabetes and heart disease.
Logistic regression was used to test the difference in ORs from GEE models and conditional logistic regression by examining the difference between the proportions of type 2 diabetes in unmatched control participants and in co-twin control participants [21,22,23,24]. Absence of a statistically significant difference in ORs from the GEE and conditional logistic regression analyses suggests that genetic and early-life familial environmental factors might not account for the observed associations. In contrast, a statistically significant difference in ORs from the GEE and conditional logistic regression analyses indicates that genetic and/or shared environmental factors likely play a role in the observed associations [15, 21,22,23,24,25].
The combined effect of the type 2 diabetes and lifestyle on heart disease risk was assessed by creating dummy variables based on the joint exposures to both factors. The presence of an additive interaction was examined by estimating the relative excess risk due to interaction (RERI), the attributable proportion (AP) and the synergy index (SI). Additionally, we examined multiplicative interaction by incorporating the two variables and their cross-product term in the same model.
Age, sex, education, BMI, smoking, alcohol consumption, marital status and physical activity were considered as potential confounders in the type 2 diabetes–heart disease association. Missing values on education (n = 1217), smoking (n = 1167), alcohol consumption (n = 1261), BMI (n = 1918), marital status (n = 755) and physical activity (n = 5938) were imputed by chained equation to obtain valid statistical inferences with five completed datasets generated. All statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA) and IBM SPSS Statistics 24.0 (IBM Corp, New York, NY, USA).
Results
Characteristics of the study population
Among all participants, 18,838 (45.4%) were men and 22,625 (54.6%) were women (χ2 = 30.95, p < 0.001). In total, 2304 (5.5%) had type 2 diabetes. Compared with type 2 diabetes-free participants, those with type 2 diabetes were more likely to be older, male, single and non-smokers; to engage in low levels of physical activity; and to have lower educational attainment and higher BMI (Table 1).
Association between type 2 diabetes and heart disease in unmatched case–control analyses
During 1998–2014, 9262 (22.3%) participants had incident heart disease. Compared with type 2 diabetes-free participants, the multi-adjusted OR for any heart disease associated with type 2 diabetes was 4.36 (95% CI 3.95, 4.81); for angina pectoris, OR 4.23 (95% CI 3.62, 4.94); for acute myocardial infarction, OR 4.93 (95% CI 4.25, 5.72); for chronic ischaemic heart disease, OR 5.14 (95% CI 3.82, 6.91); for atrial fibrillation and flutter, OR 3.14 (95% CI 2.71, 3.64); for congestive heart failure, OR 5.76 (95% CI 3.96, 8.38); and for left ventricular failure, OR 4.45 (95% CI 2.65, 7.49) (Table 2).
Association between type 2 diabetes and heart disease in co-twin control analyses
Compared with the OR in GEE models, the association between type 2 diabetes and heart disease became stronger (OR 4.89; 95% CI 3.88, 6.16) in the co-twin control analyses (including all twin pairs). The difference in ORs from the GEE models based on unmatched case–control analyses vs co-twin control analyses in all twin pairs was statistically significant (OR 1.57; 95% CI 1.42, 1.73; p < 0.001). In addition, the multi-adjusted OR (95% CI) of heart disease associated with type 2 diabetes was 4.07 (3.15, 5.27) in dizygotic twins and 10.83 (4.67, 25.10) in monozygotic twins. These results suggest that type 2 diabetes is still associated with heart disease, even after fully controlling for genetic and early-life familial environmental factors (Table 3).
Association between lifestyle-related factors and heart disease
In multi-adjusted GEE models, being a non-smoker, regular physical activity, no/mild drinking and being non-overweight were associated with a decreased risk of heart disease. In further analysis, an intermediate lifestyle and a favourable lifestyle were significantly associated with a lower risk of heart disease (Table 4).
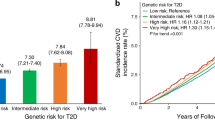
In stratified analyses by type 2 diabetes, compared with an unfavourable lifestyle, an intermediate lifestyle or a favourable lifestyle was associated with a significant 32% (OR 0.68; 95% CI 0.49, 0.93) or 56% (OR 0.44; 95% CI 0.30, 0.63) decrease in heart disease risk among patients with type 2 diabetes, respectively (Fig. 2 and electronic supplementary material [ESM] Table 1).
Joint effect of type 2 diabetes and lifestyle-related factors on heart disease risk
In joint effect analyses, there was a significant additive interaction between type 2 diabetes and lifestyle on heart disease risk (RERI 3.507; 95% CI 0.929, 6.084; AP 0.414; 95% CI 0.231, 0.597; SI 1.885; 95% CI 1.318, 2.696) (ESM Table 2). The multi-adjusted OR for type 2 diabetes multiplied by unfavourable lifestyle was 1.30 (95% CI 1.07, 1.57; p = 0.008) for heart disease.
Supplementary analysis
Considering possible sex differences in heart disease development, we performed stratified analysis, and the associations between type 2 diabetes and heart disease risk did not vary by sex (ESM Table 3). The results were not much altered compared with those from initial analyses when we repeated analyses: (1) with additional adjustment for survival status (ESM Table 4); and (2) excluding missing values for covariates (ESM Table 5).
Discussion
In this large-scale, nationwide, genetically informative sample of Swedish twins, we found that type 2 diabetes was independently associated with increased risk of heart disease and its major types, specifically angina pectoris, acute myocardial infarction, chronic ischaemic heart disease, atrial fibrillation and flutter, and heart failure. The association remained significant, even after controlling for genetic and early-life familial environmental factors. However, a healthy lifestyle might significantly mitigate the risk of heart disease related to type 2 diabetes compared with an unfavourable lifestyle.
In recent decades, many epidemiologic studies have shown that type 2 diabetes is associated with a two- to sixfold increased risk of total CVD and coronary heart disease [2, 4,5,6]. However, the association between type 2 diabetes and atrial fibrillation has been addressed in a number of epidemiologic studies with inconclusive results. Some studies showed an increased risk of atrial fibrillation among people with type 2 diabetes [8, 9, 12], but others indicated no clear association [10, 11]. In a recent meta-analysis of 32 cohort studies, type 2 diabetes was associated with a modest 30% increased atrial fibrillation risk [26]. In the present study, we found that type 2 diabetes conferred a more than fourfold greater risk of coronary heart disease and a doubled atrial fibrillation risk. Several studies have shown that type 2 diabetes is positively associated with heart failure, but in most of these the influences of other subtypes of heart disease were not taken into account [2, 27, 28]. As the onset and progression of angina pectoris, acute myocardial infarction and atrial fibrillation may also contribute to heart failure, we looked at the first onset of heart failure with no previous coronary heart disease and cardiac arrhythmias and found that the higher risk of heart failure with type 2 diabetes was independent of other specific subtypes of heart disease.
Accumulating evidence has shown that molecular defects, intrauterine environment and socioeconomic factors are associated with the development of type 2 diabetes, and also contribute to an increased risk of heart disease [13, 29]. Twins are generally raised together and share the same genetic background as well as intrauterine, childhood and adolescent environments. Twin studies provide us with an opportunity to investigate whether the association between type 2 diabetes and heart disease is potentially confounded by genetic and/or early-life familial environmental backgrounds. In the present study, results of co-twin control analyses implicate that type 2 diabetes is still associated with an increased risk of heart disease, even after fully controlling for genetic and early-life familial environmental backgrounds.
Thus far, previous studies have mainly focused on the combined effect of an overall healthy lifestyle and type 2 diabetes on mortality or total CVD (including coronary heart disease, stroke and peripheral vascular disease) risk, but data specific for only heart disease risk are limited. One population-based prospective cohort study of Chinese patients with type 2 diabetes showed that active smoking, physical inactivity, alcohol drinking and high carbohydrate intake increased the risk of all-cause mortality and CVD mortality after a mean follow-up of 4.02 years of follow-up [17]. Another prospective study including 11,527 participants with type 2 diabetes suggested that an overall healthy lifestyle (diet, smoking status, alcohol consumption and physical activity) was associated with substantially lower risks of CVD incidence (including stroke and coronary heart disease) and CVD mortality during a mean follow-up of 13.3 years of follow-up [18]. In contrast, at a median follow-up of almost 10 years, a multicentre randomised clinical trial found that an intensive lifestyle intervention (diet modification and increased physical activity) could produce improvements in CVD risk factors (such as blood pressure and high-density lipoprotein cholesterol levels) in individuals with type 2 diabetes, but not reduce CVD events (including stroke and coronary heart disease) [30]. The discrepancy in findings might reflect differences in follow-up times, lifestyle factors and definitions of outcome. To the best of our knowledge, the current study is the first to provide evidence that a healthy lifestyle consisting of being a non-smoker, no/mild alcohol consumption, regular physical activity and being non-overweight may greatly attenuate the risk of heart disease in type 2 diabetes. In the current study, patients with type 2 diabetes who reported maintaining not only a favourable (four healthy lifestyle factors) but also an intermediate lifestyle (any two or three healthy lifestyle factors) had a significantly lower heart disease risk than those with an unfavourable lifestyle (no or only one healthy lifestyle factor).
The mechanisms responsible for the increased heart disease morbidity attributable to type 2 diabetes are multifactorial and incompletely understood. An important role of metabolic disturbances, such as long-term hyperglycaemia, insulin resistance and dyslipidaemia, has been hypothesised [31, 32]. Accelerated atherosclerosis and thrombosis in patients with type 2 diabetes principally result from inflammation, reactive oxygen species and endothelial dysfunction combined with coagulation, platelet abnormalities and impaired fibrinolysis [33]. Type 2 diabetes leads to autonomic dysfunction and structural remodelling of the left atrium in the form of atrial dilatation and interstitial fibrosis, which might contribute to life-threatening arrhythmias [26]. In addition, how a favourable lifestyle mitigates the risk of heart disease among participants with or without type 2 diabetes may be explained by multiple possible mechanisms—an overall healthy lifestyle can improve glycaemic control, insulin sensitivity, blood pressure, platelet function, lipid profile and body composition [16, 17, 34].
There are several strengths and limitations in the current study. First, the large, nationwide, population-based twin cohort provided us with a unique opportunity to further examine the effect of type 2 diabetes on heart disease risk while controlling for some unmeasured confounders such as genetic and early-life familial environmental factors. Second, we used GEE modelling, which is more appropriate than logistic regression models in case–control design, since it accounts for the clustering of twins within a pair. Nonetheless, the limitations in our study need to be pointed out. First, blood glucose level was not available in the STR or SALT. Consequently, given the higher prevalence of undiagnosed type 2 diabetes in elderly people [35], subjects with undiagnosed type 2 diabetes might have been misclassified as type 2 diabetes-free, which might have led to an underestimation of the observed associations. Second, type 2 diabetes and heart disease were associated with mortality risk, which may contribute to under- or over-estimation of the observed associations. In the current study, we repeated the analyses with an additional adjustment for survival status, and the results were not substantially altered. Third, because information on lifestyle factors was obtained at baseline, it is difficult to capture potential variations in lifestyle factors during follow-up, which would result in underestimation for the effect. Fourth, although some lifestyle-related factors such as smoking, alcohol consumption and physical activity were taken into account, information on diet, sleep duration and other lifestyle-related factors was not available. Finally, information bias might have occurred due to self-reported information on lifestyle-related factors. This might have caused non-differential misclassification leading to underestimation for the observed association.
Conclusions
In conclusion, our study provides further evidence that type 2 diabetes is associated with about fourfold greater risk of heart disease, including coronary heart disease, cardiac arrhythmias and heart failure. Moreover, the association between type 2 diabetes and heart disease remains statistically significant, even after fully controlling for genetic and early-life familial environmental background. Patients with type 2 diabetes who reported maintaining a healthy lifestyle consisting of being a non-smoker, no/mild alcohol consumption, regular physical activity and being non-overweight had a significantly lower heart disease risk than those with an unfavourable lifestyle. Our findings highlight the importance of a healthy lifestyle in prevention of heart disease among patients with type 2 diabetes.
Data availability
Raw data are available by request from qualified investigators applying to the Swedish Twin Registry.
Abbreviations
- AP:
-
Attributable proportion
- GEE:
-
Generalised estimating equation
- NPR:
-
National Patient Registry
- RERI:
-
Relative excess risk due to interaction
- SALT:
-
Screening Across the Lifespan Twin study
- SI:
-
Synergy index
- STR:
-
Swedish Twin Registry
References
Grant PJ, Cosentino F (2019) The 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 40:3215–3217. https://doi.org/10.1093/eurheartj/ehz687
Shah AD, Langenberg C, Rapsomaniki E et al (2015) Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol 3:105–113. https://doi.org/10.1016/S2213-8587(14)70219-0
Benjamin EJ, Virani SS, Callaway CW et al (2018) Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation 137:E67–E492. https://doi.org/10.1161/Cir.0000000000000558
Almdal T, Scharling H, Jensen JS, Vestergaard H (2004) The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Arch Intern Med 164:1422–1426. https://doi.org/10.1001/archinte.164.13.1422
Yusuf S, Hawken S, Ounpuu S et al (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364:937–952. https://doi.org/10.1016/S0140-6736(04)17018-9
The Emerging Risk Factors Collaboration (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Cosentino F, Ceriello A, Baeres FMM et al (2019) Addressing cardiovascular risk in type 2 diabetes mellitus: a report from the European Society of Cardiology Cardiovascular Roundtable. Eur Heart J 40:2907–2919. https://doi.org/10.1093/eurheartj/ehy677
Guo Y, Tian Y, Wang H, Si Q, Wang Y, Lip GYH (2015) Prevalence, incidence, and lifetime risk of atrial fibrillation in China: new insights into the global burden of atrial fibrillation. Chest 147:109–119. https://doi.org/10.1378/chest.14-0321
Huxley RR, Lopez FL, Folsom AR et al (2011) Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 123:1501–1508. https://doi.org/10.1161/CIRCULATIONAHA.110.009035
Knuiman M, Briffa T, Divitini M et al (2014) A cohort study examination of established and emerging risk factors for atrial fibrillation: the Busselton Health Study. Eur J Epidemiol 29:181–190. https://doi.org/10.1007/s10654-013-9875-y
Rosengren A, Hauptman PJ, Lappas G, Olsson L, Wilhelmsen L, Swedberg K (2009) Big men and atrial fibrillation: effects of body size and weight gain on risk of atrial fibrillation in men. Eur Heart J 30:1113–1120. https://doi.org/10.1093/eurheartj/ehp076
Schoen T, Pradhan AD, Albert CM, Conen D (2012) Type 2 diabetes mellitus and risk of incident atrial fibrillation in women. J Am Coll Cardiol 60:1421–1428. https://doi.org/10.1016/j.jacc.2012.06.030
Langenberg C, Araneta MR, Bergstrom J, Marmot M, Barrett-Connor E (2007) Diabetes and coronary heart disease in Filipino-American women: role of growth and life-course socioeconomic factors. Diabetes Care 30:535–541. https://doi.org/10.2337/dc06-1403
Assimes TL (2011) Family history of heart disease: the re-emergence of a traditional risk factor. J Am Coll Cardiol 57:628–629. https://doi.org/10.1016/j.jacc.2010.09.036
Kato K, Sullivan PF, Evengard B, Pedersen NL (2006) Premorbid predictors of chronic fatigue. Arch Gen Psychiatry 63:1267–1272. https://doi.org/10.1001/archpsyc.63.11.1267
Marwick TH, Hordern MD, Miller T et al (2009) Exercise training for type 2 diabetes mellitus: impact on cardiovascular risk: a scientific statement from the American Heart Association. Circulation 119:3244–3262. https://doi.org/10.1161/CIRCULATIONAHA.109.192521
Lin CC, Li CI, Liu CS et al (2012) Impact of lifestyle-related factors on all-cause and cause-specific mortality in patients with type 2 diabetes: the Taichung Diabetes Study. Diabetes Care 35:105–112. https://doi.org/10.2337/dc11-0930
Liu G, Li Y, Hu Y et al (2018) Influence of lifestyle on incident cardiovascular disease and mortality in patients with diabetes mellitus. J Am Coll Cardiol 71:2867–2876. https://doi.org/10.1016/j.jacc.2018.04.027
Lichtenstein P, De Faire U, Floderus B, Svartengren M, Svedberg P, Pedersen NL (2002) The Swedish Twin Registry: a unique resource for clinical, epidemiological and genetic studies. J Intern Med 252:184–205. https://doi.org/10.1046/j.1365-2796.2002.01032.x
Carlsson S, Ahlbom A, Lichtenstein P, Andersson T (2013) Shared genetic influence of BMI, physical activity and type 2 diabetes: a twin study. Diabetologia 56:1031–1035. https://doi.org/10.1007/s00125-013-2859-3
Xu W, Qiu C, Gatz M, Pedersen NL, Johansson B, Fratiglioni L (2009) Mid- and late-life diabetes in relation to the risk of dementia: a population-based twin study. Diabetes 58:71–77. https://doi.org/10.2337/db08-0586
Bao C, Pedersen NL, Yang R et al (2018) Diabetes in midlife and risk of cancer in late life: a nationwide Swedish twin study. Int J Cancer 143:793–800. https://doi.org/10.1002/ijc.31365
Bao C, Yang R, Pedersen NL et al (2019) Overweight in midlife and risk of cancer in late life: a nationwide Swedish twin study. Int J Cancer 144:2128–2134. https://doi.org/10.1002/ijc.32005
Yang R, Pedersen NL, Bao C et al (2019) Type 2 diabetes in midlife and risk of cerebrovascular disease in late life: a prospective nested case–control study in a nationwide Swedish twin cohort. Diabetologia 62:1403–1411. https://doi.org/10.1007/s00125-019-4892-3
Xu WL, Atti AR, Gatz M, Pedersen NL, Johansson B, Fratiglioni L (2011) Midlife overweight and obesity increase late-life dementia risk: a population-based twin study. Neurology 76:1568–1574. https://doi.org/10.1212/WNL.0b013e3182190d09
Aune D, Feng T, Schlesinger S, Janszky I, Norat T, Riboli E (2018) Diabetes mellitus, blood glucose and the risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Diabetes Complicat 32:501–511. https://doi.org/10.1016/j.jdiacomp.2018.02.004
He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK (2001) Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med 161:996–1002. https://doi.org/10.1001/archinte.161.7.996
Gottdiener JS, Arnold AM, Aurigemma GP et al (2000) Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 35:1628–1637 https://doi.org/10.1016/s0735-1097(00)00582-9
Adams JN, Cox AJ, Freedman BI, Langefeld CD, Carr JJ, Bowden DW (2013) Genetic analysis of haptoglobin polymorphisms with cardiovascular disease and type 2 diabetes in the Diabetes Heart Study. Cardiovasc Diabetol 12:31. https://doi.org/10.1186/1475-2840-12-31
Look ARG, Wing RR (2010) Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med 170:1566–1575. https://doi.org/10.1001/archinternmed.2010.334
Low Wang CC, Hess CN, Hiatt WR, Goldfine AB (2016) Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus – mechanisms, management, and clinical considerations. Circulation 133:2459–2502. https://doi.org/10.1161/CIRCULATIONAHA.116.022194
Mazzone T, Chait A, Plutzky J (2008) Cardiovascular disease risk in type 2 diabetes mellitus: insights from mechanistic studies. Lancet 371:1800–1809. https://doi.org/10.1016/S0140-6736(08)60768-0
Berry C, Tardif JC, Bourassa MG (2007) Coronary heart disease in patients with diabetes. Part I: recent advances in prevention and noninvasive management. J Am Coll Cardiol 49:631–642. https://doi.org/10.1016/j.jacc.2006.09.046
Moe B, Eilertsen E, Nilsen TI (2013) The combined effect of leisure-time physical activity and diabetes on cardiovascular mortality: the Nord-Trondelag Health (HUNT) cohort study, Norway. Diabetes Care 36:690–695. https://doi.org/10.2337/dc11-2472
Gregg EW, Cadwell BL, Cheng YJ et al (2004) Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the U.S. Diabetes Care 27:2806–2812. https://doi.org/10.2337/diacare.27.12.2806
Acknowledgements
We are grateful to all the twins who took part in the study and to the members of the survey teams. The Swedish Twin Registry is managed by Karolinska Institutet and receives funding through the Swedish Research Council under grant no. 2017-00641.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
Open access funding provided by Karolinska Institute. This work was supported by the Swedish Research Council (no. 2017-00981), the National Natural Science Foundation of China (no. 81771519), the Konung Gustaf V:s och Drottning Victorias Frimurare Foundation (no. 2016-2017), Demensfonden, Strokefonden, Cornells Stiftelse and Alzheimerfonden (2017-2018). This project is part of CoSTREAM (www.costream.eu) and received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 667375.
Author information
Authors and Affiliations
Contributions
RY and WX had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. WX and XQ were involved in study concept and design. RY and HX did the statistical analysis and drafted the manuscript. NLP was involved in acquisition of data and had full access to all the data in the study. XL, JY and CB contributed to analysis and interpretation of data. All authors contributed to critical revision of the manuscript for important intellectual content. WX obtained funding for the study. WX and XQ were involved in study supervision. All authors gave their final approval of the version to be published.
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM
(PDF 140 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, R., Xu, H., Pedersen, N.L. et al. A healthy lifestyle mitigates the risk of heart disease related to type 2 diabetes: a prospective nested case–control study in a nationwide Swedish twin cohort. Diabetologia 64, 530–539 (2021). https://doi.org/10.1007/s00125-020-05324-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-020-05324-z