Abstract
Aims/hypothesis
Adiponectin is an adipokine with insulin-sensitising and anti-atherogenic properties. Several reports suggest that genetic variants in the adiponectin gene are associated with circulating levels of adiponectin, insulin sensitivity and type 2 diabetes risk. Recently two receptors for adiponectin have been cloned. Genetic studies have yielded conflicting results on the role of these genes and type 2 diabetes predisposition. In this study we aimed to evaluate the potential role of genetic variation in these genes in syndromes of severe insulin resistance, type 2 diabetes and in related metabolic traits in UK Europid populations.
Materials and methods
Exons and splice junctions of the adiponectin receptor 1 and 2 genes (ADIPOR1; ADIPOR2) were sequenced in patients from our severe insulin resistance cohort (n=129). Subsequently, 24 polymorphisms were tested for association with type 2 diabetes in population-based type 2 diabetes case–control studies (n=2,127) and with quantitative traits in a population-based longitudinal study (n=1,721).
Results
No missense or nonsense mutations in ADIPOR1 and ADIPOR2 were detected in the cohort of patients with severe insulin resistance. None of the 24 polymorphisms (allele frequency 2.3–48.3%) tested was associated with type 2 diabetes in the case–control study. Similarly, none of the polymorphisms was associated with fasting plasma insulin, fasting and 2-h post-load plasma glucose, 30-min insulin increment or BMI.
Conclusions/interpretation
Genetic variation in ADIPOR1 and ADIPOR2 is not a major cause of extreme insulin resistance in humans, nor does it contribute in a significant manner to type 2 diabetes risk and related traits in UK Europid populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adiponectin, encoded by the gene ADIPOQ (also known as 30-kDa adipocyte complement-related protein, Acrp30, APM-1, APM1, ACDC, and gelatin-binding protein-28 or GBP28), is an adipokine with insulin-sensitising [1, 2] and anti-atherogenic actions [3]. Its levels correlate strongly with insulin sensitivity in humans and animal models, and increasing levels of plasma adiponectin produce a sensitising effect to the biological action of insulin [4]. Several genetic reports have detected association between adiponectin gene variants and obesity, insulin resistance, type 2 diabetes, and adiponectin levels [5–9].
Recently, two adiponectin receptors were identified, adiponectin receptor 1 (ADIPOR1), cloned from a human skeletal muscle expression library, and adiponectin receptor 2 (ADIPOR2), identified using computational tools by Yamauchi et al. [10]. In mice, Adipor1 is expressed ubiquitously, with higher levels in skeletal muscle, and has a higher affinity for the globular form of adiponectin. Adipor2, on the other hand, is most abundant in the liver and preferentially binds the full-length form of adiponectin [10]. In contrast, both human ADIPOR1 (375aa) and ADIPOR2 (311aa) were predominantly expressed in skeletal muscle [10, 11].
In Mexican Americans, glucose-tolerant individuals with a family history of type 2 diabetes were reported to exhibit significantly lower levels of mRNA for ADIPOR1 and ADIPOR2 in skeletal muscle than subjects without a family history of diabetes. mRNA levels of both receptors were also reported to positively correlate with glucose disposal [11]. It is possible therefore that lower expression or altered function of the receptors would predispose to increased insulin resistance and type 2 diabetes. In fact, common variants in the ADIPOR1 gene were recently tested for association in a case–control study with white and African American individuals, but no association was reported [12]. Two additional studies have evaluated the role of adiponectin receptor variants and risk of type 2 diabetes. In the Old Order Amish population, two intronic variants in ADIPOR1 were reported to associate with risk of type 2 diabetes, while in ADIPOR2 an extended haplotype block was associated with increased risk of disease [13]. In contrast, in a Japanese population no associations between polymorphisms in adiponectin receptor genes and risk of type 2 diabetes were detected [14]. More recently, studies in French and Finnish populations reported no association between ADIPOR1 single nucleotide polymorphisms (SNPs) and type 2 diabetes [15, 16], although evidence for association between rs767870 in ADIPOR2 and type 2 diabetes in a French population has been suggested [15]. In light of these studies, and the potential role of these receptors in insulin action and diabetes, we sought to identify and investigate the effects of genetic variants in these genes in UK populations.
Subjects and methods
Participants
Severe insulin resistance cohort
A cohort of human patients with severe insulin resistance (SIR cohort) was collected at the University of Cambridge, UK. The inclusion criteria for this cohort were: (1) fasting insulin >150 pmol/l or exogenous insulin requirement >200 U/day; (2) acanthosis nigricans; and (3) BMI <33 kg/m2. In the present study, 129 patients from this cohort were screened for mutations in exons and splice junctions of ADIPOR1 and ADIPOR2 genes. Cambridge Local Research Ethics Committee approval was obtained, and informed consent was received from all individuals before participation.
Cambridgeshire Case–Control Study
The Cambridgeshire Case–Control Study has been described previously [17]. Briefly, this population-based case–control study consists of 552 type 2 diabetes patients and matched control subjects. DNA was available from 516 cases and control subjects for this study. The cases were a random sample of Europid men and women with type 2 diabetes, aged 47 to 75 years, from a population-based diabetes register in a geographically defined region in Cambridgeshire, UK. The presence of type 2 diabetes in these participants was defined as onset of diabetes after the age of 30 years without use of insulin therapy in the first year after diagnosis. The control participants were individually matched to each of the diabetic subjects by age, sex and geographical location, but not by BMI. Potential control subjects with HbA1c levels greater than 6% were excluded, as this subgroup could have contained a higher proportion of individuals with previously undiagnosed diabetes. Ethical approval for the study was granted by the Cambridge Local Research Ethics Committee.
EPIC-Norfolk participants
This is a nested case–control study within the EPIC-Norfolk prospective cohort study; both the case–control and full cohort study [18, 19] have been described in detail previously. Briefly, the case–control study consists of 417 incident type 2 diabetes cases and two sets of 417 control subjects, matched on age, sex, time in study and family physician, with the second set additionally matched for BMI. A case was defined by a physician’s diagnosis of type 2 diabetes, with no insulin prescribed within the first year after diagnosis, and/or HbA1c >7% at baseline or the follow-up health check. Controls were selected from those in the cohort who had not reported diabetes, cancer, stroke or myocardial infarction at baseline, and who had not developed diabetes by the time of selection. Potential control subjects with measured HbA1c levels >6% were excluded. DNA was available for this analysis from 354 cases and 741 control subjects. Ethical approval for the study was granted by the Norwich Local Research Ethics Committee.
Ely Study
This is a population-based cohort study of the aetiology and pathogenesis of type 2 diabetes and related metabolic disorders in the UK [20]. It uses an ethnically homogeneous Europid population, in which phenotypic data were recorded at the outset and after 4.5 years. The cohort was recruited from a population sampling frame with a high response rate (74%), making it representative of the general population for this area in Eastern England. This analysis included 1,721 men and women, aged 35–79 years and without diagnosed diabetes, who attended the study clinic for a health check between 2000 and 2004. Of these, 1,005 were attending a follow-up health check, while the remaining 716 were newly recruited in 2000 from the original population sampling frame. Participants attending the health check underwent standard anthropometric measurements and a 75-g oral glucose tolerance test. Plasma glucose was measured using the hexokinase method. Plasma insulin was measured by two-site immunometric assays with either 125I or alkaline phosphatase labels. Cross-reactivity with intact proinsulin was less than 0.2% and interassay CVs were less than 7%. Ethical approval for the study was granted by the Cambridge Local Research Ethics Committee.
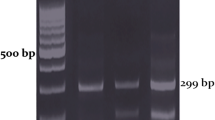
PCR and sequencing
Genomic DNA from patients was randomly preamplified in a GenomiPhi reaction (GE Healthcare UK, Chalfont St. Giles, UK) prior to amplification with gene-specific primers. Primers were designed using Primer3 software [21] to cover all coding exons and splice junctions. PCR primers and expected product sizes are described in Electronic supplementary material (ESM) Table 1. Following PCR, performed using standard conditions, products were purified using exonuclease I and shrimp alkaline phosphatase (USB Corporation, Cleveland, OH, USA), and bi-directional sequencing was performed using a DNA sequencing kit (Big Dye Terminator 3.1; Applied Biosystems, Foster City, CA, USA). Sequencing reactions were run on ABI3700 capillary machines (Applied Biosystems) and sequences were analysed using Mutation Surveyor version.2.20 (SoftGenetics LLC, State College, PA, USA).
Genotyping
SNP selection
All SNPs with a minor allele frequency greater than 2% in our SIR cohort were selected for genotyping. To increase coverage in areas not re-sequenced, a number of dbSNPs were selected in an attempt to eliminate gaps, between genotyped SNPs, of greater than 2.5–3 kb on average (additional SNPs were selected prior to HapMap phase I data release). SNP choice was based on the following criteria: (1) all putative non-synonymous SNPs in dbSNP were selected irrespective of whether or not there was frequency or validation information for the SNP; (2) SNPs with frequency information were selected if their minor allele frequency was greater than or equal to 5%; (3) for SNPs with no frequency information the choice was based on whether the SNP was a double-hit SNP, had been validated by-cluster or by-submitter; and finally (4) some SNPs with no validation information were included to try and eliminate gaps of greater than 2.5–3 kb between SNPs selected for genotyping.
Genotyping and quality control
Samples were arrayed on 96-well plates with three replicates and one water control per plate. For the case–control populations, cases and control samples were randomly distributed across each 96-well plate, with approximately the same number of cases and controls per plate. Genotyping of samples was performed in 384-well plates at the Wellcome Trust Sanger Institute, Cambridge, using an adaptation of the homogenous MassExtend protocol for the MassArray system (Sequenom, San Diego, CA, USA) [22]. Assay results for case–control are described in ESM Table 2. The following criteria were used to pass assays resulting from genotyping: (1) call rates had to be greater than or equal to 90% (in one case a call rate of 88% was accepted); (2) concordance rates between duplicate samples had to be greater than or equal to 98%; (3) minor allele frequency had to be greater than or equal to 1% in the genotyped populations; (4) agreement with Hardy–Weinberg equilibrium was tested separately in cases and controls using a χ2 goodness-of-fit test, and if p < 0.01 in controls, the assay was failed, while if p < 0.01 in cases, the assay was flagged but included in primary analysis. Assays that failed quality control were excluded from further analysis. In total we analysed results from nine SNPs in ADIPOR1 and 15 SNPs from ADIPOR2.
Statistical analysis
All analyses used SAS 8.02 (SAS Institute, Cary, NC, USA) or Stata 7.0 (Stata Corporation, College Station, TX, USA) statistical programs, unless otherwise stated. All used genotypes were in Hardy–Weinberg equilibrium. The pair-wise linkage disequilibrium (LD) coefficient for the controls (r2) was calculated for genotyped SNPs and is represented in Fig. 1. For each SNP, two primary models were used to assess association with diabetes and quantitative traits, the linear trend (additive model) on 1df and the general model on 2df. Since the results from these analyses were not materially different, we present only the results from the linear trend test. Tests for association were performed by logistic regression combined in the two case–control populations adjusting for age, sex and population. Between-study heterogeneity was tested by log-likelihood ratio tests. Quantitative trait analysis was undertaken in the Ely Study population. Association between fasting plasma insulin, fasting and 2-h post-load plasma glucose, 30-min insulin increment (30-min insulin minus fasting insulin over 30-min glucose in an OGTT), BMI and genotype was tested in a multiple regression model, adjusted for age and sex.
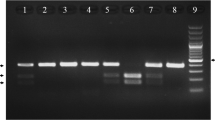
Genomic structure and pair-wise marker LD in ADIPOR1 (a) and ADIPOR2 (b). The location of SNPs identified in this study and/or genotyped is represented along the gene (bold type: SNPs selected for genotyping, and failed or monomorphic SNPs). Exons are represented in boxes (black for coding and open for untranslated). Introns and flanking sequences appear as lines. The pair-wise marker LD measured by r 2 statistics is shown below the genomic structures and indicated by the shade of grey blocks (white to black) and the r 2 value. a, b, isoforms a and b in ADIPOR2
Results
To evaluate whether genetic variation in ADIPOR1 and ADIPOR2 contributed to severe insulin resistance in humans, we sequenced exons and splice junctions in both genes in 129 individuals from our SIR cohort. These individuals were unrelated and had a variety of syndromes of severe insulin resistance [23]. We identified 13 and 29 polymorphisms in ADIPOR1 and ADIPOR2 respectively, none of which altered the protein sequence of either gene (ESM Table 3). This suggests that no functional mutations were identified in these genes. We next tested whether common variants at these genes impacted on type 2 diabetes predisposition or related quantitative traits in UK Europid populations. We selected all variants with a minor allele frequency greater than 2% in the SIR cohort and supplemented our SNP selection with additional variants from the dbSNP database plus SNPs with significant association results in other published studies. Thirteen polymorphisms from ADIPOR1 and 23 polymorphisms from ADIPOR2 were selected for genotyping in two type 2 diabetes case–control studies (n=2,127) and one metabolic quantitative trait study (n=1,721) (Fig. 1). Those SNPs that passed our genotyping quality control criteria (described in methods) were used to investigate the degree of LD in control individuals across ADIPOR1 and ADIPOR2. In total nine SNPs in ADIPOR1 and 15 SNPs in ADIPOR2 were included in the analysis. LD was measured by r 2 statistic and is depicted in Fig. 1. Under both general and linear trend models no evidence was found for statistically significant associations between SNPs and disease risk (Table 1). In ADIPOR1, SNPs rs2275738, rs2275735 and rs10581 were removed from the quantitative trait analysis as they were out of Hardy–Weinberg equilibrium (p<0.01). For the remaining SNPs there was also no evidence for association of the SNPs tested with BMI, fasting and 2-h glucose levels, fasting insulin or 30-min insulin incremental response (ESM Table 4). In ADIPOR2 a few SNPs showed nominally significant association with BMI and 2-h glucose levels. However, these results are likely to be chance findings given the number of statistical tests performed (ESM Table 4).
Discussion
The current study, including sequencing of 129 patients with syndromes of severe insulin resistance and genotyping of both population-based type 2 diabetes case–control studies (n=2,127) and a metabolic quantitative trait study (n=1,721), suggests that ADIPOR1 and ADIPOR2 genetic variants are unlikely to be major risk factors for type 2 diabetes and insulin resistance in UK Europid populations.
Although sequencing of ADIPOR1 and ADIPOR2 genes in a cohort of patients with syndromes of severe insulin resistance (n=129) led to the identification of 42 polymorphisms, including 21 novel rare variants, none altered the protein sequence. Given that this group of patients comprises a heterogeneous cohort representative of a variety of syndromes of extreme insulin resistance, the lack of variants affecting the protein sequence suggests that functional mutations in the genes ADIPOR1 and ADIPOR2 are not major causes of extreme insulin resistance in humans.
For ADIPOR1, our data in case–control studies are consistent with previous reports showing that SNPs in this gene are not associated with type 2 diabetes risk in Europid [12, 15, 16], African [12] or Japanese populations [14]. This is in contrast to evidence from the Old Order Amish, where an association of rs2275738 (and rs2275737 which is in perfect LD with it) and rs1342387 with type 2 diabetes risk has been reported [13]. Since the Amish represent an isolated population, it is possible that variants in ADIPOR1 play a role in type 2 diabetes predisposition among them, which is not apparent in more heterogeneous populations. However, given that both reported associated SNPs are present in all populations, it is unlikely that either is the true causal variant, although they could be detecting, through LD, the effect of an untested SNP. Alternatively, given the relative small sample sizes used and lack of adjustment for multiple testing, the authors may have reported a false–positive association.
For ADIPOR2 the data are less consistent. While no evidence of association between ADIPOR2 SNPs and type 2 diabetes was present in a Japanese population [14], an association has been suggested between SNP rs767870 and type 2 diabetes risk in French populations [15]. Our data, and those from the Old Order Amish [13], do not support this finding. Notably, in the French population, meta-analysis of rs767870, including 1,380 individuals with type 2 diabetes and 1,496 controls, demonstrated allelic association of nominal significance only (p=0.02), while the most significant result was under a recessive model (p=0.0018). Our study has only 23% power to detect such small recessive effects (odds ratio 1.3) with an allele frequency of 0.15, and this could explain our discrepant result. Further large scale studies of this SNP in additional populations will be required to elucidate its role in conferring risk of disease. A haplotype was also reported to increase risk of diabetes in the Old Order Amish [13]. However, when we performed haplotype analyses in both ADIPOR1 and ADIPOR2, we were unable to detect any significant associations with diabetes risk (data not shown), and this discrepancy might also be accounted for by differences in the populations studied.
With regard to quantitative metabolic traits, to date two studies have reported nominally significant results with insulin sensitivity and body size [16, 24]. The first study showed nominally significant associations between two tightly linked SNPs (rs6666089 and an intronic –1927 SNP) in ADIPOR1 and decreased insulin sensitivity and increased HbA1c levels [24]. We did not test association with HbA1c, but have not replicated any association with insulin sensitivity (including with SNP rs6666089) as assessed by fasting insulin measurements. Recently Kantartzis and colleagues reported that the association between rs6666089 and insulin sensitivity is observed only in more obese, but not in lean individuals [25]. This dependence on the degree of adiposity could explain some of the discrepant results observed for this SNP, if there are substantial differences in mean BMI between populations tested. To explore this hypothesis, we performed SNP×BMI interaction tests (using BMI both as a continuous trait and splitting the population above and below the median) on all ADIPOR1 SNPs tested. Our data provided no evidence for such an interaction (data not shown). We also specifically tested for association between rs6666089, and measures of insulin and glucose in participants with BMI above and below 25. Again we found no statistically significant difference between the two groups (p>0.3). Therefore, it is unlikely that BMI differences between populations are at the root of our discrepant results. Of note, our data cannot exclude possible small effects of this SNP on insulin sensitivity, in particular if this effect is only observed in subjects with higher BMI. The second study suggested there was evidence of association between two markers (rs10920534 and rs2275738) and BMI, but this evidence came from men only. Furthermore, three other markers (rs10920534, rs12045862 and rs7539542) were reported to associate with fasting and 2-h insulin levels, particularly in men at baseline [16]. We did not test rs10920534, but did test rs6666089 (D′=r 2=1 with rs10920534) and found no evidence for SNP×sex interaction on any of the quantitative traits we analysed. Our data also did not replicate the sex effect of SNP rs7539542 on insulin measurements. Although we did not test SNP rs12045862, previously published data was conflicting. Thus while the C allele was suggested to be associated with higher 2-h insulin levels in men (p=0.027), in women the T allele was associated with higher levels (p=0.029) [16]. Given that neither we, nor others [24], have found evidence for sex×SNP interaction effects on measures of insulin sensitivity, we suggest that further confirmatory studies are required to test this hypothesis.
Until recently, remaining uncertainty regarding the identity of the true physiological receptors for adiponectin [26] had hampered interpretation of the functional relevance of polymorphisms in ADIPOR1 and ADIPOR2 with respect to adiponectin’s insulin sensitising effects. However, a recent yeast two-hybrid screen identified an ADIPOR1 interacting molecule, APPL1, thought to mediate many of the effects of adiponectin [27]. This molecule was shown to interact with both ADIPOR1 and ADIPOR2 in an adiponectin-sensitive manner, and was shown to mediate many of adiponectin’s insulin-sensitising effects. This suggests that ADIPOR1 and ADIPOR2 could be therapeutic targets for drug development and should renew interest in association studies, such as those we present here, testing polymorphisms in ADIPOR1 and ADIPOR2 for effects on type 2 diabetes risk and metabolic traits.
In summary, sequencing of ADIPOR1 and ADIPOR2 genes in a cohort of patients with syndromes of severe insulin resistance (n=129) suggests that functional mutations in these genes are not a major cause of extreme insulin resistance in humans. Furthermore, testing of common genetic variants (n=24) did not find evidence for association of these genes with type 2 diabetes risk (n=2,127) or with five additional quantitative metabolic traits (n=1,721). These data suggest that ADIPOR1 and ADIPOR2 variants are unlikely to be major risk factors for type 2 diabetes and insulin resistance in UK Europid populations, although more detailed analyses of gene variants may be required to exclude a potential minor role of these genes in insulin resistance and glucose homeostasis.
Abbreviations
- ADIPOR1 :
-
adiponectin receptor 1
- ADIPOR2 :
-
adiponectin receptor 2
- LD:
-
linkage disequilibrium
- SIR:
-
severe insulin resistance (cohort)
- SNP:
-
single nucleotide polymorphism
References
Berg AH, Combs TP, Du X, Brownlee M, Scherer PE (2001) The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 7:947–953
Yamauchi T, Kamon J, Minokoshi Y et al (2002) Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 8:1288–1295
Ouchi N, Kihara S, Arita Y et al (2001) Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 103:1057–1063
Yamauchi T, Kamon J, Waki H et al (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941–946
Hara K, Boutin P, Mori Y et al (2002) Genetic variation in the gene encoding adiponectin is associated with an increased risk of type 2 diabetes in the Japanese population. Diabetes 51:536–540
Menzaghi C, Ercolino T, Di Paola R et al (2002) A haplotype at the adiponectin locus is associated with obesity and other features of the insulin resistance syndrome. Diabetes 51:2306–2312
Vasseur F, Helbecque N, Dina C et al (2002) Single-nucleotide polymorphism haplotypes in the both proximal promoter and exon 3 of the APM1 gene modulate adipocyte-secreted adiponectin hormone levels and contribute to the genetic risk for type 2 diabetes in French Caucasians. Hum Mol Genet 11:2607–2614
Gibson F, Froguel P (2004) Genetics of the APM1 locus and its contribution to type 2 diabetes susceptibility in French Caucasians. Diabetes 53:2977–2983
Qi L, Li T, Rimm E et al (2005) The +276 polymorphism of the APM1 gene, plasma adiponectin concentration, and cardiovascular risk in diabetic men. Diabetes 54:1607–1610
Yamauchi T, Kamon J, Ito Y et al (2003) Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423:762–769
Civitarese AE, Jenkinson CP, Richardson D et al (2004) Adiponectin receptors gene expression and insulin sensitivity in non-diabetic Mexican Americans with or without a family history of type 2 diabetes. Diabetologia 47:816–820
Wang H, Zhang H, Jia Y et al (2004) Adiponectin receptor 1 gene (ADIPOR1) as a candidate for type 2 diabetes and insulin resistance. Diabetes 53:2132–2136
Damcott CM, Ott SH, Pollin TI et al (2005) Genetic variation in adiponectin receptor 1 and adiponectin receptor 2 is associated with type 2 diabetes in the Old Order Amish. Diabetes 54:2245–2250
Hara K, Horikoshi M, Kitazato H et al (2005) Absence of an association between the polymorphisms in the genes encoding adiponectin receptors and type 2 diabetes. Diabetologia 48:1307–1314
Vaxillaire M, Dechaume A, Vasseur-Delannoy V et al (2006) Genetic analysis of ADIPOR1 and ADIPOR2 candidate polymorphisms for type 2 diabetes in the Caucasian population. Diabetes 55:856–861
Siitonen N, Pulkkinen L, Mager U et al (2006) Association of sequence variations in the gene encoding adiponectin receptor 1 (ADIPOR1) with body size and insulin levels. The Finnish Diabetes Prevention Study. Diabetologia 49:1795–1805
Barroso I, Luan J, Middelberg RP et al (2003) Candidate gene association study in type 2 diabetes indicates a role for genes involved in beta-cell function as well as insulin action. PLoS Biol 1:E20
Harding AH, Day NE, Khaw KT et al (2004) Dietary fat and the risk of clinical type 2 diabetes: the European Prospective Investigation of Cancer—Norfolk study. Am J Epidemiol 159:73–82
Day N, Oakes S, Luben R et al (1999) EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer 80 (Suppl 1):95–103
Williams DR, Wareham NJ, Brown DC et al (1995) Undiagnosed glucose intolerance in the community: the Isle of Ely Diabetes Project. Diabet Med 12:30–35
Rozen S, Skaletsky H (2000) Primer3 on the WWW for general users and for biologist programmers. Methods Mol Biol 132:365–386
Whittaker P, Bumpstead S, Downes K, Ghori J, Deloukas P (2006) SNP analysis by MALDI-TOF mass spectrometry. In: Celis J, Carter N, Simons K, Small JV, Hunter T (eds) Cell biology: a laboratory handbook, 3rd edn. Academic, San Diego
Barroso I, Gurnell M, Crowley VE et al (1999) Dominant negative mutations in human PPARgamma associated with severe insulin resistance, diabetes mellitus and hypertension. Nature 402:880–883
Stefan N, Machicao F, Staiger H et al (2005) Polymorphisms in the gene encoding adiponectin receptor 1 are associated with insulin resistance and high liver fat. Diabetologia 48:2282–2291
Kantartzis K, Fritsche A, Machicao F, Haring HU, Stefan N (2006) The -8503 G/A polymorphism of the adiponectin receptor 1 gene is associated with insulin sensitivity dependent on adiposity. Diabetes Care 29:464
Hug C, Wang J, Ahmad NS, Bogan JS, Tsao TS, Lodish HF (2004) T-cadherin is a receptor for hexameric and high-molecular-weight forms of Acrp30/adiponectin. Proc Natl Acad Sci USA 101:10308–10313
Mao X, Kikani CK, Riojas RA et al (2006) APPL1 binds to adiponectin receptors and mediates adiponectin signalling and function. Nat Cell Biol 8:516–523
Acknowledgements
We thank S. Bumpstead for genotyping support. I. Barroso is funded by the Wellcome Trust. S. O’Rahilly and I. Barroso acknowledge support from EU FP6 funding (contract no. LSHM-CT-2003-503041). The EPIC-Norfolk study is funded by MRC UK and Cancer Research UK. The MRC Ely Study is funded by the MRC and Wellcome Trust (to N. J. Wareham). We are grateful to all patients, volunteers, referring physicians and staff of the SIR, Cambridgeshire Case–Control, EPIC-Norfolk, and MRC Ely studies.
Duality of interest
The authors declare that no conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table 1
Primer sequences and PCR product sizes used for sequencing ADIPOR1 and ADIPOR2 (DOC 46 kb)
Table 2
Genotyping assay results for case-control studies (DOC 61 kb)
Table 3
SNPs detected by sequencing ADIPOR1 and ADIPOR2 in severely insulin-resistant patients (DOC 78 kb)
Table 4
ADIPOR1 and ADIPOR2 SNP association results with quantitative traits (DOC 215 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Collins, S.C., Luan, J., Thompson, A.J. et al. Adiponectin receptor genes: mutation screening in syndromes of insulin resistance and association studies for type 2 diabetes and metabolic traits in UK populations. Diabetologia 50, 555–562 (2007). https://doi.org/10.1007/s00125-006-0534-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0534-7