Abstract
OBJECTIVE: To describe primary care physicians’ clinical decision making regarding late-life depression.
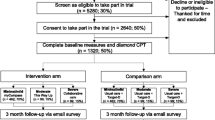
DESIGN: Longitudinal collection of data regarding physicians’ clinical assessments and the volume and content of patients’ ambulatory visits as part of a randomized clinical trial of a physician-targeted intervention to improve the treatment of late-life depression.
SETTING: Academic primary care group practice.
PATIENTS/PARTICIPANTS: One-hundred and eleven primary care physicians who completed a structured questionnaire to describe their clinical assessments immediately following their evaluations of 222 elderly patients who had reported symptoms of depression on screening questionnaires.
EVTERVENTIONS: Intervention physicians were provided with their patient’s score on the Hamilton Depression rating scale (HAM-D) and patient-specific treatment recommendations prior to completing the questionnaire regarding their clinical assessment.
MAIN RESULTS: Those physicians not provided HAM-D scores were just as likely to rate their patients as depressed, as determined by specific query of these physicians regarding their clinical assessments. A physician’s clinical rating of likely depression did not consistently result in the formulation of treatment intentions or actions. Treatment intentions and actions were facilitated by provision of treatment algorithms, but treatment was received by fewer than half of the patients whom physicians intended to treat. Barriers to treatment appear to include both physician and patient doubts about treatment benefits.
CONCLUSIONS: Lack of recognition of depressive symptoms did not appear to be the primary barrier to treatment. Recognition of symptoms and access to treatment algorithms did not consistently result in progression to subsequent stages in treatment decision making. More research is needed to determine how patients and physicians weigh the potential risks and benefits of treatment and how accurately they make these judgments.
Similar content being viewed by others
References
Moore JT, Siliemperi DR, Bobula JA. Recognition of depression by family medicine residents. J Fam Pract. 1978;7:509–13.
Seller RH, Blascovich J, Lenkel E. Influence of stereotypes in the diagnosis of depression by family practice residents. J Fam Pract. 1981;12:849–54.
Zung WWK, Magill M, Moore JT, George DT. Recognition and treatment of depression in a family medicine practice. J Clin Psychiatry. 1983;44:3–6.
Kessler LG, Cleary PD, Burke JD Jr. Psychiatric disorders in primary care: results of a follow-up study. Arch Gen Psychiatry. 1985;42:583–7.
Schulberg HC. Saul M, McClelland M, Ganguli M, Christy W, Frank R. Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry. 1985;42:1164–70.
Jones L, Badger L, Ficken R, Leeper JD, Anderson RL. Inside the hidden mental health delivery of primary care physicians. Gen Hosp Psychiatry. 1987;9:287–93.
Marks J, Goldberg D, Hitter V. Determinants of the ability of general practitioners to detect psychiatric illness. Psychol Med. 1979;9:337.
Von Korff M, Shapiro S, Burke JD, et al. Anxiety and depression in a primary care clinic. Arch Gen Psychiatry. 1987;44:152–6.
German PS, Shapiro S, Skinner EA, et al. Detection and management of mental health problems of older patients by primary care providers. JAMA. 1987;257(4):489–93.
Shapiro S, German PS, Skinner EA, et al. An experiment to change detection and management of mental morbidity in primary care. Med Care. 1987;25:327–39.
Gerber PD, Barrett J, Manheimer E, Whiting R, Smith R. Recognition of depression by internists in primary care. J Gen Intern Med. 1989;4:7–13.
Waxman HM, Carner EA. Physician’s recognition, diagnosis, and treatment of mental disorders in elderly medical patients. Gerontologist. 1984;24(6):593–97.
Johnstone A, Goldberg D. Psychiatric screening in general practice: a controlled trial. Lancet. 1976;1:605.
Linn LS, Yager J. The effect of screening, sensitization, and feedback on notation of depression. J Med Educ. 1980;55:942–9.
Zung WWK, King RE. Identification and treatment of masked depression in a general medical practice. J Clin Psychiatry. 1983;44:365–8.
Hoeper EW, Nycz GR, Kessler LG, et al. The usefulness of screen-Ing for mental illness. Lancet. 1984;2:33–5.
Rucker L, Frye EB, Cygan RW. Feasibility and usefulness of depression screening in medical outpatients. Arch Intern Med. 1986;146:729–31.
Rand EH, Badger LW, Coggins DR. Toward a resolution of contradictions. Utility of feedback from the GHQ. Gen Hosp Psych. 1988;10:189–96.
Magruder-Habib K, Zung WWK, Feussner JR. Improving physicians’ recognition and treatment of depression in general medical care. Med Care. 1990;28:239–50.
Brody DS, Lerman CE, Wolfson HG, Caputo GC. Improvement in physicians’ counseling of patients with mental health problems. Arch Intern Med. 1990;150:993–8.
Katon W, Von Korff M, Lin E, et al. A randomized trial of psychiatric consultation with distressed high utilizers. Gen Hosp Psychiatry. 1992;14:86–98.
Callahan CM, Hendrie HC, Dittus RS, Brater DC, Hui SL, Tierney WM. Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc. 1994;42:839–46.
Schulberg HC, McClelland M, Coulehan JL, Block M, Werner G. Psychiatric decision making in family practice: future research directions. Gen Hosp Psychiatry. 1986;8:1–6.
Katon W, Kleinman A, Rosen G. Depression and somatization. Am J Med. 1982;72:127–35, 241–7.
Rapp SR, Davis KM. Geriatric depression: physicians’ knowledge, perceptions, and diagnostic practices. Gerontologist. 1989;29(2):252–57.
Callahan CM, Nienaber NA, Hendrie HC, Tierney WM. Depression of elderly outpatients: primary care physicians’ attitudes and practice patterns. J Gen Intern Med. 1992;7:26–31.
Williamson P, Beitman BD, Katon W. Beliefs that foster physician avoidance of psychosocial aspects of health care. J Fam Pract. 1981;13:999–1003.
Ford CV, Sbordone RJ. Attitudes of psychiatrists toward elderly. Am J Psychiatry. 1980;137:571–5.
Goldberg DP, Steele J, Johnson A, Smith C. Ability of primary care physicians to make accurate ratings of psychiatric symptoms. Arch Gen Psychiatry. 1982;39:829–33.
Steinberg H, Torem M, Saravay SM. An analysis of physician resistance to psychiatric consultations. Arch Gen Psychiatry. 1980;37:1007–12.
Ouslander JG. Physical illness and depression in the elderly. J Am Geriatr Soc. 1982;30:593–9.
McGreevey JF Jr. Franco K. Depression in the elderly: the role of the primary care physician in management. J Gen Intern Med. 1988;3:498–507.
Orleans CT, George LK, Houpt JL, Brodie HKH. How primary care physicians treat psychiatric disorders: a national survey of family practitioners. Am J Psychiatry. 1985;142(1):52–7.
Tierney WM, Miller ME, Hui SL, McDonald CJ. Practice randomization and clinical research. The Indiana experience. Med Care. 1991;29:JS57–64.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–41.
Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3.
Hamilton M. A rating scale for depression. J Neurol Neursurg Psychiatry. 1960;23:56–62.
Bergner M, Bobbit RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19:787–805.
McDonald CM. Tierney WM, Martin DK, Overhage JM. The Regenstrief Medical Record System: 20 years of experience in hospital outpatient clinics and neighborhood health centers. MD Comput 1992;9:206–17.
Daniels ML, Linn LS, Ward N, Leake B. A study of physician preferences in the management of depression in the general medical setting. Gen Hosp Psychiatry. 1986;8:229–35.
Roskin G, Marell SK. Differences in attitudes toward patients among medical specialties. Int J Psychiatry Med. 1988;18(3):223–33.
Coryell W. Shifts in attitudes among psychiatric residents: serial measures over 10 years. Am J Psychiatry. 1987;144(7):913–7.
Badger LW, Rand EH. Unlearning psychiatry: a cohort effect in the training environment. Int J Psychiatry Med. 1988;18(2):123–35.
Weinberger M, Cohen SJ, Mazzuca SA. The role of physicians’ knowledge and attitudes in effective diabetes management. Soc Sci Med. 1984;9:965–9.
Dietrich AJ, Goldberg H. Preventive content of adult primary care. Do generalists and subspecialists differ? Am J Public Health. 1984;74:223–7.
Author information
Authors and Affiliations
Additional information
Supported in part by a grant from the John A. Hartford Foundation, New York, New York. Dr. Callahan was supported by grant K08 AG00538-02 from the National Institutes of Health, Dr. Tierney was supported by grants HS07632, HS07763, and HSO7719 from the Agency for Health Care Policy and Research.
The opinions expressed herein are solely those of the authors and not necessarily those of the supporting institutions and agencies.
Rights and permissions
About this article
Cite this article
Callahan, C.M., Dittus, R.S. & Tierney, W.M. Primary care physicians’ medical decision making for late-life depression. J Gen Intern Med 11, 218–225 (1996). https://doi.org/10.1007/BF02642478
Issue Date:
DOI: https://doi.org/10.1007/BF02642478