Abstract
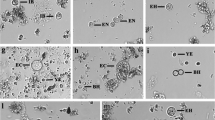
The use of sodium acetate acetic acid formalin (SAF)-preserved stool specimens was compared with that of nonpreserved specimens for the recovery of intestinal protozoa. A total of 247 patients, 170 with diarrhea of more than one week's duration and 77 refugees, were asked to collect a stool specimen. Each specimen was placed into two vials, one empty, the other containing SAF fixative. Laboratory investigations included microscopic examination of the concentrated sediment and direct wet smears from both types of stool specimens and the microscopic examination of a permanent stained smear from the unsedimented, SAF-preserved stool specimens. Examination of SAF-preserved stool specimens revealed intestinal protozoa in 149 of the 247 patients. With the conventional procedure using unpreserved stool specimens, intestinal protozoa were found in 89 of the 247 patients. The results show that the examination of SAF-preserved stool specimens, consisting of the microscopic examination of both the concentrated sediment and the permanent stained smear from the unsedimented material, increases the chance of recovering intestinal protozoa as compared to the conventional procedure.
Similar content being viewed by others
References
Mank TG, Zaat JOM, Polderman AM: Underestimation of intestinal protozoa as a cause of diarrhoea in general practice. Nederlands Tijdschrift voor Geneeskunde 1995, 139: 324–327.
Polderman AM, Rijpstra AC: Medische parasitologie, handleiding bij de laboratoriumdiagnostiek. Bonn Stafleu Van Loghum, Houten/Zaventem, 1993, p. 122–196.
Smith JW, Bartlett MS: Diagnostic parasitology: introduction and methods. In: Balows A, Hausler WJ, Herrmann KC, Isenberg HD, Shadomy HJ (ed): Manual of clinical microbiology. American Society for Microbiology, Washington DC, 1991, p. 701–716.
Garcia LS, Bruckner DA: Diagnostic medical parasitology. American Society for Microbiology, Washington DC, 1993, p. 501–540.
Garcia LS, Shimizu RY: Medical parasitology update on diagnostic techniques and laboratory safety. Laboratory Medicine 1993, 24: 81–88.
Parasitology Subcommittee/Microbiology Section of Scientific Assembly: Recommended procedures for the examination of clinical specimens submitted for the diagnosis of parasitic infections. American Journal of Medical Technology 1978, 44: 1101–1106.
Wolfe MS: Giardiasis. Clinical Microbiology Reviews 1992, 5: 93–100.
Garcia LS, Shimizu RY, Brewer AC, Bruckner DA: Evaluation of intestinal parasite morphology of copper sulfate and mercuric chloride bases for use in Schaudinn fixative. Journal of Clinical Microbiology 1983, 17: 1092–1095.
Yang J, Scholten T: A fixative for intestinal parasites permitting the use of concentration and permanent staining procedures. American Journal of Clinical Pathology 1977, 67: 300–304.
Scholten T: An improved technique for the recovery of intestinal protozoa. Journal of Parasitology 1972, 58: 633–634.
Junod C: Technique coprologique nouvelle essentiellement destinée à la concentration des trophozoites d'amibes. Bulletin Societé Pathologiste Exotique 1972, 65: 390–398.
Ridley DS, Hawgood BC: The value of formol-ether concentration of fecal cysts and ova. Journal of Clinical Pathology 1956, 9: 74–76.
Palmer J: Modified iron hematoxylin/kinyoun stain. Clinical Microbiology Newsletter 1991, 13: 39–40.
Yang J, Scholten T:Dientamoeba fragilis: a review with notes on its epidemiology, pathogenicity, mode of transmission, and diagnosis. American Journal of Tropical Medicine and Hygiene 1977, 26: 16–22.
Millet V, Spencer MJ, Chapin M, Stewart M, Yatabe JA, Brewer T:Dientamoeba fragilis, a protozoan parasite in adult members of a semicommunal group. Digestive Diseases and Sciences 1983, 28: 335–339.
Casemore DP: Foodborne protozoal infection. Lancet 1990, 336: 1427–1432.
Zierdt CH: Pathogenicity ofBlastocystis hominis. Journal of Clinical Microbiology 1991, 29: 662–663.
van Gool T, Canning EU, Dankert J: An improved practical and sensitive technique for the detection of microsporidian spores in stool samples. Transactions of the Royal Society of Tropical Medicine and Hygiene 1994, 88: 189–190.
van Gool T, Hollister WS, Eeftinck Schattenkerk J, van den Bergh Weerman KM, Bartelsman MA, Bruins WM, Canning JJM, Dankert J: Diagnosis of microsporidian infections in patients with HIV by a new rapid fluorescent technique. Journal of Clinical Pathology 1993, 46: 694–699.
Casemore D, Armstrong M, Sands R: Laboratory diagnosis of cryptosporidiosis. Journal of Clinical Pathology 1985, 38: 1337–1341.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mank, T.G., Zaat, J.O.M., Blotkamp, J. et al. Comparison of fresh versus sodium acetate acetic acid formalin preserved stool specimens for diagnosis of intestinal protozoal infections. Eur. J. Clin. Microbiol. Infect. Dis. 14, 1076–1081 (1995). https://doi.org/10.1007/BF01590942
Issue Date:
DOI: https://doi.org/10.1007/BF01590942