Abstract
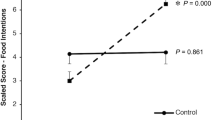
Health promotion efforts targeting nontraditional college students (older, part-time enrollment, and working) may be an optimal way to reach large populations that potentially face health disparities. A randomized trial was undertaken to examine the feasibility of a nutrition and physical activity behavioral intervention among nontraditional undergraduate college students at a large urban public university. Over 8 weeks, participants received either (1) a brief tailored feedback report plus three motivational interviewing-based calls from trained peer counselors (intervention; n = 40) or (2) the report only (control; n = 20). Participants mean age was 32 years (SD = 10), 58 % were female, 47 % were racial/ethnic minorities, and 25 % reported receiving public health insurance. Most (78 %) intervention group participants completed at least two of three peer counseling calls. At follow-up, those in the intervention vs. control group self-reported beneficial, but non-statistically significant changes in fruits and vegetables (+0.7 servings/day), sugary drinks (−6.2 oz/day), and fast food visits (−0.2 visits/week). For physical activity, there was a non-statistically significant decrease in moderate-vigorous physical activity (107.2 min/week) in the intervention vs. control group. Overall satisfaction with the program was high, although there were recommendations made for improving the structure and number of calls. Findings indicate that the intervention was feasible with promising effects on nutrition behaviors and the need to better target physical activity behaviors. Future work entails implementation in a larger sample with objectively measured behaviors.

Similar content being viewed by others
References
Ogden CL, Lamb MM, Carroll MD, Flegal KM (2010) NCHS Data Brief, No. 50: obesity and socioeconomic status in adults: United States, 2005–2008
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA J Am Med Assoc 307:491–497. doi:10.1001/jama.2012.39
Fine LJ, Philogene GS, Gramling R et al (2004) Prevalence of multiple chronic disease risk factors: 2001 national health interview survey. Am J Prev Med 27:18–24. doi:10.1016/j.amepre.2004.04.017
Kushi LH, Byers T, Doyle C et al (2006) American cancer society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 56:254–281
Laska MN, Pelletier JE, Larson NI, Story M (2012) Interventions for weight gain prevention during the transition to young adulthood: a review of the literature. J Adolesc Health 50:324–333. doi:10.1016/j.jadohealth.2012.01.016
Choy S (2002) Nontraditional undergraduates: findings from the condition of education no. NCES 2002–012. Washington DC: U.S. Department of Education, National Center for Education Statistics 2002; http://nces.ed.gov/pubs2002/2002012.pdf
Snyder T, Dillow S (2012) Digest of education statistics, 2011 chapter 3, no. NCES 2012–2001. Washington DC: U.S. Department of education, institute of education sciences, national center for education statistics. http://nces.ed.gov/pubs2012/2012001.pdf Accessed 23 January 2015
U.S. Department of Education Profile of Undergraduate Students 2007–08 no. NCES 2010–205 (2010) Washington DC: U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics. http://nces.ed.gov/pubs2010/2010205.pdf Accessed 23 January 2015
Kulavic K, Hultquist CN, McLester JR (2013) A comparison of motivational factors and barriers to physical activity among traditional versus nontraditional college students. J Am Coll Health 61:60–66. doi:10.1080/07448481.2012.753890
Sorensen G, Emmons K, Hunt MK et al (2003) Model for incorporating social context in health behavior interventions: Applications for cancer prevention for working-class, multiethnic populations. Prev Med 37:188–197. doi:10.1016/S0091-7435(03)00111-7
McNeill LH, Stoddard A, Bennett GG et al (2012) Influence of individual and social contextual factors on changes in leisure-time physical activity in working-class populations: results of the healthy directions-small businesses study. Cancer Causes Control 23:1475–1487. doi:10.1007/s10552-012-0021-z
Shelton RC, Goldman RE, Emmons KM et al (2011) An investigation into the social context of low-income, urban Black and Latina women: Implications for adherence to recommended health behaviors. Health Educ Behav 38:471–481. doi:10.1177/1090198110382502
Sorensen G, Stoddard AM, Dubowitz T et al (2007) The influence of social context on changes in fruit and vegetable consumption: Results of the healthy directions studies. Am J Public Health 97:1216–1227. doi:10.2105/AJPH.2006.088120
Office of Institutional Research and Policy Studies (2010) Headcount and FTE enrollment. Boston MA: University of Massachusetts Boston. http://cdn.umb.edu/images/oirp/2013_TABLE1-Student_Headcount__FTE_by_Full-timePart-time_Status.pdf Accessed 23 January 2015
Office of Institutional Research and Policy Studies (2008) Who are our undergraduates? Boston MA: office of institutional research and policy studies, University of Massachusetts Boston. http://www.umb.edu/editor_uploads/images/oirp/WhoareourUndergraduates_Feb-08.ppt Accessed 23 January 2015
U.S. Department of Agriculture, U.S. Department of Health and Human Services (2010) Dietary guidelines for Americans, 2010. GPO, Washington DC
Moyers T, Martin T, Manuel J, Miller (2005) The motivational interviewing treatment integrity (MITI) Code: Version 2.0
Rollnick S, Miller W, Butler C (2008) Motivational interviewing in health care: helping patients change behavior. The Guilford Press
Quintiliani L, Bishop H, Greaney M, Whiteley J (2012) Factors across home, work, and school domains influence nutrition and physical activity behaviors of nontraditional college students. Nutr Res 32:757–763
Health and Retirement Study (2008) Survey research center, institute for social research, university of Michigan national institute on aging, health and retirement study. http://hrsonline.isr.umich.edu Accessed 23 January 2015
Block G, Gillespie C, Rosenbaum EH, Jenson C (2000) A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med 18:284–288
Hedrick VE, Comber DL, Estabrooks PA et al (2010) The beverage intake questionnaire: Determining initial validity and reliability. J Am Diet Assoc 110:1227–1232. doi:10.1016/j.jada.2010.05.005
California Health Interview Survey (2009) UCLA center for health policy research; California department of public health; California department of health care services. http://healthpolicy.ucla.edu/chis/design/Pages/questionnairesEnglish.aspx Accessed 23 January 2015
Yore M, Ham S, Ainsworth B et al (2007) Reliability and validity of the instrument used in BRFSS to assess physical activity. Med Sci Sports Exerc 39:1267–1274. doi:10.1249/mss.0b013e3180618bbe
Sallis JF, Pinski RB, Grossman RM et al (1988) The development of self-efficacy scales for health related diet and exercise behaviors. Health Educ Res 3:283–292. doi:10.1093/her/3.3.283
Prochaska J, Redding C, Evers K (2008) The transtheoretical model and stages of change. Health behavior health education: theory research practice, 4th ed. San Francisco, CA: Jossey Bass, pp 97–121
Klein HJ, Wesson MJ, Hollenbeck JR et al (2001) The assessment of goal commitment: a measurement model meta-analysis. Organ Behav Hum Decis Process 85:32–55. doi:10.1006/obhd.2000.2931
Quintiliani L, Carbone E (2005) Impact of diet-related cancer prevention messages written with cognitive and affective arguments on message characteristics, stage of change, and self-efficacy. J Nutr Educ Behav 37:12–19. doi:10.1016/S1499-4046(06)60254-6
Campbell MK, Honess-Morreale L, Farrell D et al (1999) A tailored multimedia nutrition education pilot program for low-income women receiving food assistance. Health Educ Res 14:257–267. doi:10.1093/her/14.2.257
Poobalan AS, Aucott LS, Precious E et al (2010) Weight loss interventions in young people (18 to 25 year olds): a systematic review. Obes Rev 11:580–592. doi:10.1111/j.1467-789X.2009.00673.x
Greene GW, White AA, Hoerr SL et al (2012) Impact of an online healthful eating and physical activity program for college students. Am J Health Promot 27:E47–E58. doi:10.4278/ajhp.110606-QUAN-239
Pokhrel P, Little MA, Herzog TA (2014) Current methods in health behavior research among U.S. community college students a review of the literature. Eval Health Prof 37:178–202. doi:10.1177/0163278713512125
Lesley ML (2007) Social problem solving training for African Americans: effects on dietary problem solving skill and DASH diet-related behavior change. Patient Educ Couns 65:137–146
Acknowledgments
This work was supported by funding from the National Cancer Institute at the National Institutes of Health (grant number 5R03CA139943), and from the National Library of Medicine at the National Institutes of Health (grant number T15LM007092) from a post-doctoral fellowship to L.Q. The National Cancer Institute and the National Library of Medicine had no role in the design, analysis, or writing of this article. The authors acknowledge scientific mentoring provided by Robert H. Friedman, MD and Glorian Sorensen, PhD and technical assistance in data analysis provided by Heather Kelley, MA and in implementing the study protocol provided by Hillary Bishop, MPH and Nathan Brooks, MD, MPH. Finally, the authors thank the many students and staff members who supported this research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quintiliani, L.M., Whiteley, J.A. Results of a Nutrition and Physical Activity Peer Counseling Intervention among Nontraditional College Students. J Canc Educ 31, 366–374 (2016). https://doi.org/10.1007/s13187-015-0858-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-015-0858-4