Abstract
Lower urinary tract symptoms (LUTS) are commonly associated with benign prostatic hyperplasia (BPH) and represent significant bother among aging men. Bothersome LUTS secondary to BPH, including nocturia, significantly impact men’s general health-related quality of life (QoL) as do sleep disturbances. However, very few studies have examined the relationship between the severity of BPH-related urinary symptoms and sleep disturbances. This review analyzes the recent studies that report the association between the bother and severity of LUTS secondary to BPH and the severity of sleep disturbance. In addition, we address the relationship between treating LUTS and the influence that it has on treating the sleep disorders.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
McVary KT. BPH: epidemiology and comorbidities. Am J Manag Care. 2006;12:S122.
Weiss JP, Blaivas JG. Nocturia. Curr Urol Rep. 2003;4:362.
• Chartier-Kastler E, Leger D, Cornet D. Prostatic hyperplasia is highly associated with nocturia and excessive sleepiness: a cross-sectional study. BMJ Open. 2012;2(3):2012. An important recent study about the relationship between BPH and excessive sleepiness.
Donovan JL. Measuring the impact of nocturia on quality of life. BJU Int. 1999;84 Suppl 1:21.
Koseoglu H, Aslan G, Ozdemir I, et al. Nocturnal polyuria in patients with lower urinary tract symptoms and response to alpha-blocker therapy. Urology. 2006;67:1188.
• Tikkinen KA, Johnson 2nd TM, Tammela TL, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–96. An important population based study on the relationship between nocturia and QoL.
Yoshimura K, Oka Y, Kamoto T, et al. Night-time frequency, sleep disturbance and general health-related quality of life: is there a relation? Int J Urol. 2009;16:96.
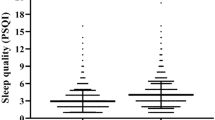
•• Helfand BT, McVary KT, Meleth S, et al. The relationship between lower urinary tract symptom severity and sleep disturbance in the CAMUS trial. J Urol. 2012;185:2223–8. A very important and the most recent study on the relationship between LUTS and sleep disorders.
Moriyama Y, Miwa K, Tanaka H, et al. Nocturia in men less than 50 years of age may be associated with obstructive sleep apnea syndrome. Urology. 2008;71:1096.
• Schneider T, de la Rosette JJ, Michel MC. Nocturia: a non-specific but important symptom of urological disease. Int J Urol. 2009;16:249. An important study on nocturia.
Weiss JP, Blaivas JG, Stember DS, et al. Nocturia in adults: etiology and classification. Neurourol Urodyn. 1998;17:467.
Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999;84:297.
Cai T, Gardener N, Abraham L, et al. Impact of surgical treatment on nocturia in men with benign prostatic obstruction. BJU Int. 2006;98:799.
Abraham L, Hareendran A, Mills IW, et al. Development and validation of a quality-of-life measure for men with nocturia. Urology. 2004;63:481.
Vaughan CP, Endeshaw Y, Nagamia Z, et al. A multicomponent behavioural and drug intervention for nocturia in elderly men: rationale and pilot results. BJU Int. 2009;104:69.
Gooren L. Androgen deficiency in the aging male: benefits and risks of androgen supplementation. J Steroid Biochem Mol Biol. 2003;85:349.
Coyne KS, Kaplan SA, Chapple CR, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int. 2009;103 Suppl 3:24.
• Lee J, Andriole G, Avins A, et al. Redesigning a large-scale clinical trial in response to negative external trial results: the CAMUS study of phytotherapy for benign prostatic hyperplasia. Clin Trials. 2009;6:628. An important study about the effects of phytotherapy on BPH.
• Wilt T, Ishani A, Stark G, et al. Serenoa repens for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2009;(2):CD001423. An important study about serenoa repens and the effects on BPH.
Boyle P, Robertson C, Lowe F, et al. Updated meta-analysis of clinical trials of Serenoa repens extract in the treatment of symptomatic benign prostatic hyperplasia. BJU Int. 2004;93:751.
Jenkins CD, Stanton BA, Niemcryk SJ, et al. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313.
Chiu YH, Silman AJ, Macfarlane GJ, et al. Poor sleep and depression are independently associated with a reduced pain threshold. Results of a population based study. Pain. 2005;115:316.
Nasermoaddeli A, Sekine M, Kumari M, et al. Association of sleep quality and free time leisure activities in Japanese and British civil servants. J Occup Health. 2005;47:384.
Helfand BT, Fought A, Manvar AM, et al. Determining the Utility of Recalled Lower Urinary Tract Symptoms. Urology. 2010 Aug;76(2):442–7.
Jolleys JV, Donovan JL, Nanchahal K, et al. Urinary symptoms in the community: how bothersome are they? Br J Urol. 1994;74:551.
Kasturi S, Russell S, McVary KT. Metabolic syndrome and lower urinary tract symptoms secondary to benign prostatic hyperplasia. Curr Urol Rep. 2006;7:288.
Kane CJ, Raheem OA, Bent S, et al. What do I tell patients about saw palmetto for benign prostatic hyperplasia? Urol Clin North Am. 2011;38:261–77.
Heland B, Lee J, McVary K, et al. Associations between improvements in lower urinary tract symptoms and sleep disturbance over time in the CAMUS trial. J Urol. (in press)
Disclosure
OO Cakir reported no potential conflicts of interest relevant to this article; KT McVary has received compensation as a consultant for Lilly, Allergan, NIDDK, Watson, and Neotract; has a grant or pending grant with Johnson & Johnson; and has lectured for GSK.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cakir, O.O., McVary, K.T. LUTS and Sleep Disorders: Emerging Risk Factor. Curr Urol Rep 13, 407–412 (2012). https://doi.org/10.1007/s11934-012-0281-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-012-0281-x