Abstract
Introduction
‘Syndromic hypermobility’ encompasses heritable connective tissue disorders such as hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders which are characterised by excessive joint range of motion and pain. Conservative interventions such as exercise are the cornerstone of management, yet their effectiveness is unclear.
Aim
To systematically appraise the effectiveness of conservative management for people with syndromic hypermobility.
Method
A systematic online database search was conducted (AMED, BND, CINAHL Plus, MEDLINE, PEDro, PsychINFO and SportDiscus). Potential articles were assessed for eligibility by two researchers against the following criteria: adults and children with a hEDS/HSD diagnosis (or equivalent diagnosis using specific criteria); non-pharmacological or non-surgical interventions; outcomes related to pain, physical function, psychological well-being or quality of life. Controlled trials and cohort studies were included. Critical Appraisal Skills Programme checklists were used to assess methodological quality.
Results
Eleven studies were included, comprising eight controlled trials and three cohort studies. All studies investigated interventions that had exercise as the primary component. Three small controlled studies demonstrated superior effects of conservative management relative to a control group. However, those studies only focused on a single area of the body, only recruited women, and had no long-term follow-up. All studies reported improvements in a wide range of outcomes over time.
Conclusion
Controlled trial evidence for the superiority of conservative management over comparators is weak. There is some evidence that people improve over time. Robust randomised controlled trial research of the long-term effectiveness of ‘whole-body’ (rather than individual joints or body areas) conservative management is required.
Key Points • Conservative management is the cornerstone of management of syndromic hypermobility. • The review found that evidence for the effectiveness of conservative management relative to no treatment or other conservative comparators was weak. • However, there was consistent evidence for effectiveness from pre- to post-treatment. • Further robust randomised controlled trial evidence is required. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
‘Hypermobility’ defines the ability of one joint or multiple joints to move beyond what might be considered a normal range of motion [1]. In some cases, hypermobility can be an asset, such as in sport and the performance arts. However, it is also a feature of heritable connective tissue disorders such as hypermobile Ehlers-Danlos syndrome (hEDS) [2] and hypermobility spectrum disorders (HSD) [1]. The terms hEDS/HSD have replaced previous diagnostic categories of Ehlers-Danlos syndrome hypermobility type (EDS-HT) (Villefranche criteria [3]) and joint hypermobility syndrome (JHS) (Brighton criteria [4]). Within this manuscript, we will refer to ‘syndromic hypermobility’ as an umbrella term to cover the new and historical diagnoses. Syndromic hypermobility is commonly associated with pain, fatigue, cycles of injury and recovery [5] in addition to a wide range of other symptoms affecting the musculoskeletal, gastrointestinal, cardiovascular and autonomic nervous systems [6]. Symptoms can have a negative impact upon strength, proprioception, function and quality of life [7]. The prevalence of the new diagnostic categories of hEDS [2] and HSD [1] have yet to be established; however, 30% of people referred to a musculoskeletal triage service in the UK met the historical Brighton criteria for JHS [8]. Similar high prevalence rates for JHS were reported for UK pain management (39.1%), rheumatology (37.0%) and orthopaedic lower limb (10.9%) clinic referrals [9]. Syndromic hypermobility is therefore likely to be more common within musculoskeletal services than traditionally believed, although it should be noted that a much smaller proportion of people are likely to meet the new stricter hEDS diagnostic criteria [2].
Syndromic hypermobility is under-recognised and poorly understood and its assessment and management are deemed complex [1]. A multidisciplinary and patient-centred approach is recommended [10]. The British Society of Paediatric and Adolescent Rheumatology [11] highlighted the ineffectiveness of current medical management for hypermobility-related pain in young children and adolescents, recommending a multi-systemic approach. Surgery should be considered as a last resort when other interventions have been unsuccessful because syndromic hypermobility patients have a higher risk of surgical complications, such as reduced effectiveness of local anaesthesia and delayed wound healing [12]. Rombaut et al. [13] reported that only 33.9% of EDS-HT patients who had surgery reported a positive effect, compared to 63.4% of those receiving physiotherapy. Care needs to be taken in interpreting those figures as the circumstances and indications for such interventions were likely to have been very different and thus they are not directly comparable. Nonetheless, it is clear that the effectiveness of conservative management in people with syndromic hypermobility warrants systematic exploration.
Previous systematic reviews in this area provided some support for the use of conservative management. For example, Smith et al. [14] explored the effectiveness of physiotherapy and occupational therapy management, Palmer et al. [15] investigated the effects of therapeutic exercise, and Peterson et al. [16] reviewed mechanical and physical interventions for lower limb symptoms specifically in children. Findings were mostly positive, with results particularly suggesting that exercise, as a component of management, can be effective in improving symptoms. However, the need for further high-quality evidence was consistently identified, with a lack of randomised controlled trial (RCT) evidence and methodological limitations of the included studies. Several more recent potentially relevant RCTs (e.g. 17, 18) and cohort studies (e.g. 19) have since been published. An updated review that explores a wider range of conservative interventions in both children and adults is therefore required.
Rombaut et al. [13] emphasised the need for evidence-based recommendations for optimal management. For healthcare professionals managing people with EDS, a lack of high-quality clinical guidelines have been reported, limiting evidence-based practice [17]. Palmer et al. [7] highlighted a lack of knowledge and understanding regarding diagnosis and management among physiotherapists. The current systematic review therefore aims to systematically identify and appraise the existing research evidence relating to the effectiveness of conservative management for syndromic hypermobility.
Methodology
The review was conducted and reported according to PRISMA guidelines [18]. The protocol was not registered with the international prospective register of systematic reviews (PROSPERO).
A librarian with systematic reviewing expertise advised on the choice of electronic databases and construction of the search strategy. The electronic databases chosen were AMED (Allied & Complementary Medicine), CINAHL Plus (Cumulative Index to Nursing & Allied Health Literature), MEDLINE, PsychINFO and SportDiscus (all via EBSCO); BND (British Nursing Database); and PEDro (Physiotherapy Evidence Database).
The research question was refined using the PICO format (Table 1) to ensure a focused and comprehensive search [19]. Consultation with the librarian led to the development of a simple and inclusive search strategy, focussing only on the ‘population’ and ‘intervention’ due to the relatively limited range of literature available in this area (Table 2).
A Boolean search strategy was used on EBSCO and BND to search for relevant articles. The ‘OR’ operation was used within each search to identify one or more terms, with ‘AND’ being used to combine the search terms [20]. Where possible within each electronic database, the search was limited to articles in the English language published from 1998 onwards. A simplified search strategy of ‘hypermobil*’ was used for PEDro to ensure the retrieval of all relevant articles. The electronic literature search was conducted on 27 February 2019 and updated on 1 June 2020.
Inclusion and exclusion criteria (Table 3) were developed a priori to reflect the PICO research question. Duplicates were removed and the remaining articles were independently evaluated by two researchers against the eligibility criteria to determine the appropriateness of titles, abstracts and full-text articles. Any disagreements between reviewers were discussed by the wider research group and agreed by consensus. All articles included for full-text review and relevant previously published systematic reviews [14,15,16] were also ‘snowballed’ by one researcher. Snowballing is the process of identifying additional research from reference lists to reduce the risk of missing preliminary evidence [23]. The articles included and excluded, with reasons, were reported according to PRISMA guidelines [18].
The methodological quality and risk of bias of the included studies was appraised using Critical Appraisal Skills Programme (CASP) checklists for RCTs [24] and cohort studies [25]. CASP checklists are recommended for group work within healthcare, ensuring succinct and effective consideration of the components needed for critical appraisal of evidence [26]. Two researchers appraised the included articles independently and then agreed a shared interpretation of the quality of each article. Any discrepancies were discussed with the wider research group until consensus was found. The results were then tabulated. Following critical appraisal, key data was extracted (including participants, sample size, location/setting, intervention, outcome measures and findings) and this was also tabulated. This informed a narrative synthesis of the findings. Meta-analysis was not attempted due to substantial heterogeneity in study design, interventions and outcome measures.
Results
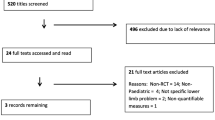
Eleven studies were included in the final review. Figure 1 outlines the process of article identification and assessment of eligibility according to PRISMA guidance [18].
Key characteristics of each of the controlled trials and cohort studies are reported in Tables 4 and 5. There were eight controlled trials (including seven RCTs and a pilot RCT) and three cohort studies (one of which was a pilot study).
Of the controlled studies, only Celenay and Kaya [29], Daman et al. [30] and Reychler et al. [35] found consistent evidence of the superiority of conservative interventions relative to no-treatment controls post-treatment. However, those studies only focused on a single area of the body, only recruited women, and had no long-term follow-up. Unfortunately, Sahin et al. [36] failed to report a direct head-to-head statistical comparison between trial arms following treatment. Two controlled studies [32, 33] reported inconsistent findings, with only parent-reported outcomes demonstrating differences between groups. For example, Pacey et al. [33] found that the parent-reported physical quality of life score favoured exercise to neutral, whilst the parent-reported psychosocial score favoured exercise into the hypermobile range. Kemp et al. [32] found that parental global assessment favoured targeted physiotherapy rather than generalised physiotherapy, but only at 5 months. None of the other child-reported or physical outcome measures reported by these studies [32, 33] differed between groups. Bale et al. [27] found no difference on any outcome between a multidisciplinary intervention and usual care. The final controlled trial [34] was clearly identified as a pilot study, aimed at informing a future definitive trial of physiotherapy. It was therefore not explicitly designed to determine the effectiveness of the intervention and, as a result, did not conduct between-group statistical analyses. In summary, the evidence for the effectiveness of conservative management relative to comparators is weak and contradictory.
There was much more consistent evidence from the controlled studies and cohort studies of positive effects of conservative management from pre- to post-treatment. This included a very wide variety of patient-reported, parent-reported and objective outcomes across impairment, activity and participation levels.
Five studies were conducted in the UK, two in Turkey, and one each in Australia, Iran and Norway. Three studies were with children [27, 32, 33], with the remainder being in adult participants. Bathen et al. [28], Celenay and Kaya [29], Daman et al. [30] and Reychler et al. [35] recruited only women, whilst the others had both sexes. Total samples sizes recruited ranged from n = 12 to n = 119, with n = 10 to n = 59 allocated to the conservative intervention groups.
The intervention duration ranged from 4 weeks to 4 months, with the final outcomes being at the end of treatment in seven of the 11 studies. Bale et al. [27] had the longest follow-up (12 months following baseline). All conservative interventions featured exercise as a core component, accompanied in some cases by a range of additional interventions such as occupational therapy [27], discussions and lectures [28] or information and advice [34]. Some interventions (and associated outcomes) were specific to a single body area such as the spine [29], inspiratory muscles [35] or the knee joint [18, 19, 30, 32, 35]. A very wide range of impairment, activity and participation level outcome measures were included across the studies.
Summaries of the CASP appraisal of each of the RCTs and cohort studies are reported in Table 6 and Table 7, respectively. Key aspects related to study quality will be discussed in the following section.
Discussion
This review aimed to determine the effectiveness of conservative management for the management of syndromic hypermobility. The included papers all used exercise as a core component of the interventions investigated. Post-treatment, there was some weak evidence for superior effects of conservative management relative to no-treatment controls [18, 28, 29], but such evidence was inconsistent or absent when compared against other forms of conservative management [27, 32, 33, 36]. All studies reported evidence of positive effects on a range of outcomes from pre- to post-treatment within the conservative intervention groups. However, the studies included in the review had a range of methodological limitations and thus the evidence needs to be interpreted with caution.
Study quality
The overall quality of the controlled studies was variable (Table 6), with identified weaknesses in relation to factors such as blinding, the comparability of groups at the start of the trial, the comparability of how groups were treated, the reporting of precision estimates, and the completeness of outcome assessment. The cohort studies also had identified weaknesses, particularly in relation to the identification of and accounting for confounding variables and the completeness and length of follow-up (Table 7). Some of the methodological limitations will now be explored in more detail.
Group allocation
Randomisation reduces systematic error and improves internal validity by ensuring that group differences following intervention are due to treatment effects and not confounding variables [38]. Random allocation also aims to reduce selection bias by distributing patient characteristics evenly between groups [39].
Randomisation was conducted in all eight of the controlled trials. Kemp et al. [32] and Celenay and Kaya [29] both used computer-generated block randomisation, whilst Daman et al. [30], Reychler et al. [35], Pacey et al. [33] and Palmer et al. [34] used simple computer-generated randomisation. Bale et al. [27] used minimisation techniques, a valid alternative to randomisation [40]. However, the study by Sahin et al. [36] lacked clarity and detail regarding the randomisation process.
Of the controlled trials, Bale et al. [27], Celenay and Kaya [29], Daman et al. [30], Kemp et al. [32] and Sahin et al. [36] reported that randomisation resulted in no significant differences between group characteristics at baseline. However, Reychler et al. [35] and Pacey et al. [33] found a difference in age and Palmer et al. [34] found a difference in age and sex between groups following randomisation.
Due to the study design, randomisation was not appropriate in the three cohort studies. Ferrell et al. [31] and Bathen et al. [28] conducted single group cohort studies, in which all participants were exposed to the same intervention, whereas To and Alexander [37] conducted a three-group cohort study (JHS, generalised joint hypermobility (GJH) and normal mobility). Cohort studies can be advantageous in collecting specific exposure data; however, they are often criticised for being vulnerable to influences from confounding variables [41].
Blinding
Six of the eight controlled trials reported blinding. Pacey et al. [33] performed a double-blind trial, with the treating therapist blinded to the results of assessment and patients blinded to the difference between the two exercise programmes. Bale et al. [27], Daman et al. [30], Celenay and Kaya [29] and Reychler et al. [35] performed single-blind studies, blinding outcome assessors to intervention groups. Kemp et al. [32] also used a single-blind method, blinding the physiotherapist delivering sessions to participant demographic data, diagnostic criteria, symptom scores, joint range, strength and fitness assessments.
Palmer et al. [34] reported being unable to blind participants or assessors due to the nature of the intervention. This is recognised as a limitation in evaluating conservative treatments [42, 43]. Blinding was not discussed or reported by Ferrell et al. [31], Sahin et al. [36], To and Alexander [37] or Bathen et al. [28].
Confounding variables
Confounding variables are external factors that affect the true relationship between an intervention (the independent variable) and the study outcome (the dependent variable) [44]. Consideration of confounding variables is particularly important in cohort studies as they reduce the internal validity of the study [45]. To and Alexander [37] recognised that pain was likely to confound their investigation, and therefore ensured that anterior knee pain was a feature of all groups. Detailed eligibility criteria were also documented, which reduces the risk that the recruited population had other confounding variables that may negatively affect the outcomes [46]. However, Bathen et al. [28] and Ferrell et al. [31] both lacked detail regarding the presence or control of confounding variables, meaning that external factors, such as comorbidities, may have influenced findings. Bathen et al. [28] reported only the demographics and characteristics of the participants, and Ferrell et al. [31] reported only their age and Beighton score. If confounding variables are not controlled for during selection, they can be accounted for during statistical analysis [46]. However, neither Bathen et al. [28] nor Ferrell et al. [31] reported doing so, limiting interpretation of their findings as the effect of the interventions may have been obscured by external factors [47].
Participants
The majority of studies used convenience sampling to recruit participants from hospital physiotherapy, rheumatology or hypermobility clinics. Convenience sampling refers to selecting participants based on accessibility; although considered the least rigorous sampling method, it is widely used within clinical research as it is easy and affordable [48, 49]. To and Alexander [37] recruited from a variety of sources, including support groups. Such sources risk recruitment of an unrepresentative sample as support group members are likely to be more compliant and proactive in managing their condition [50]. Bathen et al. [28] did not clearly state from where participants were recruited.
Clear eligibility criteria were outlined in nine studies, with the exception of Bathen et al. [28] and Ferrell et al. [31]. It is essential to consider how eligibility criteria might impact the validity of the research [51]. For example, very strict eligibility criteria can limit external validity [52]. Six of the nine studies that clearly reported eligibility criteria excluded participants that had a history of other musculoskeletal pathology, including osteoarthritis, previous surgery and ligament damage, particularly at the knee joint. The remaining three studies excluded participants based on refusal to give consent or the presence of other chronic conditions. Exclusion based on comorbidities is likely to strengthen claims of a causal path between exposure and outcome [53]. However, patients with syndromic hypermobility are at higher risk of musculoskeletal complications, chronic pain and joint degeneration [54]. Therefore, exclusion of comorbidities may create a sample that is unrepresentative, limiting external validity and clinical relevance.
Sample size and retention
Researchers use sample size calculations to determine how many participants are required to answer their research question [55]. An adequate sample size is required to detect statistically significant treatment effects [56]. Small sample sizes are vulnerable to type two statistical errors, and larger than required sample sizes risk wasting limited resources [57]. Of the eight controlled trials, only two [27, 30] performed prospective sample size calculations and then managed to recruit and retain the number of participants identified. The other six controlled trials either did not report a prospective sample size [34, 36], failed to recruit the required sample [32, 33] or recruited to the required sample but were unable to retain that number in the trial [29, 35]. Of the three cohort studies, only To and Alexander [37] recruited and retained participants in excess of a prospectively calculated sample size. The others did not report prospective sample size calculations [28, 31].
Although Bathen et al. [28], Sahin et al. [36] and Ferrell et al. [31] did not perform sample size calculations, they all found statistically significant improvements in some outcomes over time in the conservative intervention groups. Type II errors for the outcomes that did not improve over time cannot be discounted. Palmer et al. [34] did not perform a sample size calculation as it was clearly identified as a pilot study with no inferential statistical analysis. It should also be noted that a direct head-to-head statistical comparison of the intervention and control groups post-treatment was not reported by Sahin et al. [36] and thus, it is not certain if that study was powerful enough to detect such a difference.
Follow-up
Long-term follow-up is important in demonstrating effectiveness beyond the period of active therapeutic intervention, something that is of particular relevance to life-long conditions such as syndromic hypermobility. In eight of the 11 studies, the final study outcomes were completed immediately at the end of treatment, with no long-term follow-up at all. The longest follow-up was observed in Bale et al. [27] who assessed patients at 3-month (only 6% attrition) and 12-month post-intervention (12% attrition). Completeness of follow-up is an important determinant of validity [58]. Attrition rates were generally low, with only two of the included studies exceeding 30% attrition (33% [34] and 44% [32]).
Outcome measures
A very wide range of outcome measures were explored, incorporating impairment, activity and participation. This is important as it evidences the comprehensive effects of the interventions investigated. Ten of the 11 studies investigated pain intensity. With the exception of Bathen et al. [28] and Palmer et al. [34], all reported statistically significant improvements in pain intensity from pre- to post-treatment.
Strengths and limitations of the review
Key strengths of the review were the very robust search strategy, and the group processes for identifying, screening and critically appraising studies. The two reviewers experienced less agreement when using the CASP cohort study checklist than with the RCT checklist. This led to more discussion with the wider research group to agree an interpretation of those studies. Whilst this consensus might be seen as a strength, the interpretation and application of the cohort study checklist may still be open to debate. It should be acknowledged that only three of the studies included were with children, thereby limiting the application of findings to paediatric syndromic hypermobility populations. All studies included exercise as a core component of the interventions evaluated and thus the effectiveness of other conservative interventions is unknown.
Clinical implications
This review provides valuable insight into the potential impacts of conservative management in syndromic hypermobility. Inspiratory muscle training [35], spinal stabilisation exercises [29] and a combined exercise programme (closed kinetic chain exercises and proprioception exercises) [30] all demonstrated effects that were superior to no-treatment controls. However, no clear recommendations can be made about the superiority of particular types of conservative interventions over other conservative management approaches.
Although positive findings were reported in the included studies, it is important to consider the intensity of the interventions and how well these might be integrated into healthcare delivery. For example, two of the three RCTs that demonstrated superior effects of exercise over no-treatment controls [29, 30, 35] both used rather intensive interventions. In Daman et al. [30], patients attended 3 days per week for 4 weeks, supervised by an expert physiotherapist, and in Celenay and Kaya [29], patients attended 3 days per week for 8 weeks, again supervised by an experienced physiotherapist (although that intervention was delivered as a group programme). It remains to be seen whether less therapist-intensive interventions, which employ a greater emphasis on supported self-management, can demonstrate clinical effectiveness within the context of an RCT. Interventions such as that piloted by Palmer et al. [34] might translate more easily into clinical practice as they match common physiotherapy delivery patterns, at least within a UK context [7]. Such self-management approaches are coherent with recommendations for long-term conditions [59] and enhancing capability to self-manage has been associated with lower healthcare utilisation [60].
Recommendations for future research
Further rigorous RCTs are required. Other recommendations for future research include ensuring a priori sample size calculations; employing effective blinding and randomisation techniques to reduce the risk of bias; selecting outcome measures that capture the multidimensional impact of syndromic hypermobility; and investigating ‘whole body’ management (rather than individual joints or body areas), including conservative management approaches other than exercise.
Conclusion
This systematic review provides weak evidence for the effectiveness of conservative management for the management of syndromic hypermobility. This is based on three small RCTs (n = 20–46) that demonstrated superior effects relative to no treatment on outcomes such as joint position sense, muscle endurance, pain, physical function and postural stability. However, those studies only recruited women, focused on a single area of the body and had no long-term follow-up. The review found no evidence for superior effects of specific conservative interventions when compared with other such interventions. All studies (including cohort studies) observed improvements from pre- to post-treatment in adults and children in a very wide range of impairment, activity and participation level outcomes. The reviewed evidence related to interventions that had exercise as a core component.
Evidence included in the review should be interpreted with caution due to a range of methodological limitations. There remains a need for more rigorous randomised controlled studies to better inform clinical practice. Future studies should pay particular attention to issues related to sample size, blinding, long-term follow-up, the evaluation of ‘whole body’ management (rather than individual joints or body areas) and the inclusion of adequate comparators.
References
Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A (2017) A framework for the classification of joint hypermobility syndrome and related conditions. Am J Med Genet C: Semin Med Genet 175(1):148–157. https://doi.org/10.1002/ajmg.c.31539
Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, Bloom L, Bowen JM, Brady AF, Burrows NP, Castori M, Cohen H, Colombi M, Demirdas S, De Backer J, De Paepe A, Fournel-Gigleux S, Frank M, Ghali N, Giunta C, Grahame R, Hakim A, Jeunemaitre X, Johnson D, Juul-Kristensen B, Kapferer-Seebacher I, Kazkaz H, Kosho T, Lavallee ME, Levy H, Mendoza-Londono R, Pepin M, Pope FM, Reinstein E, Robert L, Rohrbach M, Sanders L, Sobey GJ, Van Damme T, Vandersteen A, van Mourik C, Voermans N, Wheeldon N, Zschocke J, Tinkle B (2017) The 2017 international classification of the Ehlers-Danlos syndromes. AmJ Med Genet C: Semin Med Genet 175(1):8–26. https://doi.org/10.1002/ajmg.c.31552
Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ (1998) Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Am J Med Genet 77:31–37. https://doi.org/10.1002/(sici)1096-8628(19980428)77:1<31::aid-ajmg8>3.0.co;2-o
Grahame R, Bird HA, Child A (2000) The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol 27(7):1777–1779
Terry R, Palmer S, Rimes K, Clark C, Simmonds J, Horwood J (2015) Living with joint hypermobility syndrome. Patient experiences of diagnosis, referral and self-care. Fam Pract 32(3):354–358. https://doi.org/10.1093/fampra/cmv026
Tinkle B, Castori M, Berglund B, Cohen H, Grahame R, Kazkaz H, Levy H (2017) Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome type III and Ehlers-Danlos syndrome hypermobility type): clinical description and natural history. Am J Med Genet Part C Semin Med Genet 175C:48–69. https://doi.org/10.1002/ajmg.c.31538
Palmer S, Cramp F, Lewis R, Muhammad S, Clark E (2015) Diagnosis, management and assessment of adults with joint hypermobility syndrome: a UK wide survey of physiotherapy practice. Musculoskeletal Care 13:101–111. https://doi.org/10.1002/msc.1091
Connelly E, Hakim E, Davenport S, Simmonds J (2014) A study exploring the prevalence of joint hypermobility syndrome in patients attending a musculoskeletal triage clinic. Physiother Pract Res 36(1):43–53. https://doi.org/10.3233/PPR-140046
To M, Simmonds J, Alexander C (2017) Where do people with joint hypermobility syndrome present in secondary care? The prevalence in a general hospital and the challenges of classification. Musculoskeletal Care 15(1:3–9. https://doi.org/10.1002/msc.1147
Simmonds J, Keer R (2008) Hypermobility and the hypermobility syndrome, part 2: assessment and management of hypermobility syndrome. Man Ther 13(2):1–11. https://doi.org/10.1016/j.math.2007.11.001
British Society for Paediatric and Adolescent Rheumatology (BSPAR) (2012) Guidelines for management of joint hypermobility syndrome in children and young people. Available from: https://www.sparn.scot.nhs.uk/wp-content/uploads/2017/01/Guidelines-for-Management-of-Joint-Hypermobility-Syndrome-v1.1-June-2013.pdf [Accessed 13 March 2020]
Hashemi-Nejad A, Vanhegan I (2016) Ehlers-Danlos support UK - orthopaedic surgery in hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders. Available from: https://www.ehlers-danlos.org/information/orthopaedic-surgery-in-hypermobile-ehlers-danlos-syndrome-and-hypermobility-spectrum-disorders [Accessed 13 March 2020]
Rombaut L, Malfait F, de Wandele I, Cools A, Thijs Y, de Paepe A, Calders P (2011) Medication, surgery, and physiotherapy among patients with the hypermobility type of Ehlers-Danlos syndrome. Arch Phys Med Rehabil 92(7):1106–1112. https://doi.org/10.1016/j.apmr.2011.01.016
Smith T, Bacon H, Jerman E, Easton V, Armon K, Poland F, Macgregor AJ (2014) Physiotherapy and occupational therapy interventions for people with benign joint hypermobility syndrome: a systematic review of clinical trials. Disabil Rehabil 36(10):797–803. https://doi.org/10.3109/09638288.2013.819388
Palmer S, Bailey S, Barker L, Barney L, Elliott A (2014) The effectiveness of therapeutic exercise for joint hypermobility syndrome: a systematic review. Physiotherapy 100:220–227. https://doi.org/10.1016/j.physio.2013.09.002
Peterson B, Coda A, Pacey V, Hawke F (2018) Physical and mechanical therapies for lower limb symptoms in children with hypermobility spectrum disorder and hypermobile Ehlers-Danlos syndrome: a systematic review. J Foot Ankle Res 11(1):1–11. https://doi.org/10.1186/s13047-018-0302-1
Sulli A, Talarico R, Scire CA, Avcin T, Castori M, Ferraris A, Frank C, Grunert J, Paolino S, Bombardieri S, Schneider M, Smith V, Cutolo M, Mosca M, Malfait F (2018) Ehlers-Danlos syndromes: state of the art on clinical practice guidelines. RMD Open 4(S1):e000790. https://doi.org/10.1136/2Frmdopen-2018-000790
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Methley A, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comprehensive study of the specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14(579):1–10. https://doi.org/10.1186/s12913-014-0579-0
Ecker E, Skelly A (2010) Conducting a winning literature search. Evid Based Spine Care J 1(1):9–14. https://doi.org/10.1055/2Fs-0028-1100887
Marnach M, Ramin K, Ramsey P, Song S, Stensland J, An K (2003) Characterization of the relationship between joint laxity and maternal hormones in pregnancy. Obstet Gynecol 101(2):331–335. https://doi.org/10.1016/s0029-7844(02)02447-x
Norton P, Baker J, Sharp H, Warenski J (1995) Genitourinary prolapse and joint hypermobility in women. Obstet Gynecol 85(2):225–228. https://doi.org/10.1016/0029-7844(94)00386-R
Callahan J (2014) Writing literature reviews: a reprise and update. Hum Resour Dev Rev 13(3):271–275. https://doi.org/10.1177/2F1534484314536705
Critical Appraisal Skills Programme (2018) CASP randomised controlled checklist. Available at: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Randomised-Controlled-Trial-Checklist-2018.pdf [Accessed 13 March 2020]
Critical Appraisal Skills Programme (2018) CASP cohort study checklist. Available at: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Cohort-Study-Checklist_2018.pdf [Accessed 13 March 2020]
Nadelson S, Nadelson L (2014) Evidence-based practice article reviews using CASP tools: a method for teaching EBP. Worldviews Evid-Based Nurs 11(5):344–346. https://doi.org/10.1111/wvn.12059
Bale P, Easton V, Bacon H, Jerman E, Watts L, Barton G, Clark A, Armon K, MacGregor A (2019) The effectiveness of a multidisciplinary intervention strategy for the treatment of symptomatic joint hypermobility in childhood: a randomised, single centre parallel group trial (the Bendy study). Pediatr Rheumatol Online J 17(2):1–10. https://doi.org/10.1186/s12969-018-0298-x
Bathen T, Hangmann AB, Hoff M, Anderson LO, Rand-Hendriksen S (2013) Multidisciplinary treatment of disability in Ehlers-Danlos syndrome hypermobility type/hypermobility syndrome: a pilot study using a combination of physical and cognitive-behavioral therapy on 12 women. Am J Med Genet A 161A(12):3005–3011. https://doi.org/10.1002/ajmg.a.36060
Celenay S, Kaya D (2017) Effects of spinal stabilization exercises in women with benign joint hypermobility syndrome: a randomized controlled trial. Rheumatol Int 37(9):1461–1468. https://doi.org/10.1007/s00296-017-3713-6
Daman M, Shiravani F, Hemmati L, Taghizadeh S (2019) The effect of combined exercise therapy on knee proprioception, pain intensity and quality of life in patients with hypermobility syndrome: a randomized clinical trial. J Bodyw Mov Ther 23(1):202–205. https://doi.org/10.1016/j.jbmt.2017.12.012
Ferrell W, Tennant N, Sturrock R, Ashton L, Creed G, Brydson G, Rafferty D (2004) Amelioration of symptoms by enhancement of proprioception in patients with joint hypermobility syndrome. Arthritis Rheum 50(10):3323–3328. https://doi.org/10.1002/art.20582
Kemp S, Roberts I, Gamble C, Wilkinson S, Davidson J, Baildam E, Cleary A, McCann L, Beresford M (2010) A randomized comparative trial of generalized vs targeted physiotherapy in the management of childhood hypermobility. Rheumatology (Oxford) 49(2):315–325. https://doi.org/10.1093/rheumatology/kep362
Pacey V, Tofts L, Adams R, Munns C, Nicholson L (2013) Exercise in children with joint hypermobility syndrome and knee pain: a randomised controlled trial comparing exercise into hypermobile versus neutral knee extension. Pediatr Rheumatol Online J 11(1):30. https://doi.org/10.1186/1546-0096-11-30
Palmer S, Cramp F, Clark E, Lewis R, Brookes S, Hollingworth W, Welton N, Thom H, Terry R, Rimes KS, Horwood J (2016) The feasibility of a randomised controlled trial of physiotherapy for adults with joint hypermobility syndrome. Health Technol Assess 20(47):1–264. https://doi.org/10.3310/hta20470
Reychler G, Liistro G, Piérard GE, Hermanns-Lê T, Manicourt D (2019) Inspiratory muscle strength training improves lung function in patients with the hypermobile Ehlers–Danlos syndrome: a randomized controlled trial. Am J Med Genet A 179A:356–364. https://doi.org/10.1002/ajmg.a.61016
Sahin N, Baskent A, Cakmak A, Salli A, Ugurlu H, Berker E (2008) Evaluation of knee proprioception and effects of proprioception exercise in patients with benign joint hypermobility syndrome. Rheumatol Int 28(10):995–1000. https://doi.org/10.1007/s00296-008-0566-z
To M, Alexander C (2018) Are people with joint hypermobility syndrome slow to strengthen? Arch Phys Med Rehabil 100(7):1243–1250. https://doi.org/10.1016/j.apmr.2018.11.021
Fives A, Russell D, Kearns N, Lyons R, Eaton P, Canavan J, Devaney C, O'Brien A (2013) The role of random allocation in randomized controlled trials: distinguishing selection bias from baseline imbalance. J Multidiscip Eval 9(20):33–42 http://journals.sfu.ca/jmde/index.php/jmde_1/article/view/371
Akobeng A (2005) Understanding randomised controlled trials. Arch Dis Child 90(8):840–844. https://doi.org/10.1136/2Fadc.2004.058222
Bland J, Altman D (2011) Comparisons against baseline within randomised groups are often used and can be highly misleading. Trials 12:264. https://doi.org/10.1186/1745-6215-12-264
Song J, Chung K (2010) Observational studies: cohort and case-control studies. Plast Reconstr Surg 126(6):2234–2242. https://doi.org/10.1097/2FPRS.0b013e3181f44abc
Boutron I, Guittet L, Estellat C, Moher D, Hrobjartsson A, Ravaud P (2007) Reporting methods of blinding in randomised controlled trials assessing non-pharmacological treatments. PLoS Med 4(2):e61. https://doi.org/10.1371/journal.pmed.0040061
Hrobjartsson A, Emanuelsson F, Thomsen A, Hilden J, Brorson S (2014) Bias due to lack of patient blinding in clinical trials. A systematic review of trials randomizing patients to blind and nonblind sub-studies. Int J Epidemiol 43(4):1272–1283. https://doi.org/10.1093/ije/dyu115
Skelly A, Dettori J, Brodt E (2012) Assessing bias: the importance of considering confounding. Evid Based Spine Care J 3(1):9–12. https://doi.org/10.1055/2Fs-0031-1298595
Bookwala A, Hussain N, Bhandari M (2011) The three-minute appraisal of a prospective cohort study. Indian J Orthop 45(4):291–293. https://doi.org/10.4103/2F0019-5413.80315
Garg R (2016) Methodology for research. Indian J Anaesth 60(9):640–645. https://doi.org/10.4103/2F0019-5049.190619
Jager K, Zoccali C, MacLeod A, Dekker F (2008) Confounding: what it is and how to deal with it. Kidney Int 73(3):256–260. https://doi.org/10.1038/sj.ki.5002650
Elfil M, Negida A (2017) Sampling methods in clinical research: an educational review. Emerg (Tehran) 5(1):e52 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5325924/
Marshall M (1996) Sampling for qualitative research. Fam Pract 13(6):522–526. https://doi.org/10.1093/fampra/13.6.522
Fraser S, Spink K (2002) Examining the role of social support and group cohesion in exercise compliance. J Behav Med 25(3):233–249. https://doi.org/10.1023/a:1015328627304
Patino C, Ferreira J (2018) Inclusion and exclusion criteria in research studies: definitions and why they matter. J Bras Pnemol 44(2):84. https://doi.org/10.1590/2FS1806-37562018000000088
Rothwell P (2006) Factors that can affect the external validity of randomised controlled trials. PLOS Clin Trials 1(1):e9. https://doi.org/10.1371/2Fjournal.pctr.0010009
Infante-Rivard C, Cusson A (2018) Reflection on modern methods: selection bias – a review of recent developments. Int J Epidemiol 47(5):1714–1722. https://doi.org/10.1093/ije/dyy138
Malfait F, Hakim A, de Paepe A, Grahame R (2006) The genetic basis of the joint hypermobility syndromes. Rheumatology (Oxford) 45(5):502–507. https://doi.org/10.1093/rheumatology/kei268
Jones S, Carley S, Harrison M (2003) An introduction to power and sample size estimation. Emerg Med J 20(5):453–458. https://doi.org/10.1136/2Femj.20.5.453
Hickey G, Grant S, Dunning J, Siepe M (2018) Statistical primer: sample size and power calculations – why, when, and how? Eur J Cardiothorac Surg 54(1):4–9. https://doi.org/10.1093/2Fejcts%2Fezy169
Nayak B (2010) Understanding the relevance of sample size calculation. Indian J Ophthalmol 58(6):469–470. https://doi.org/10.4103/2F0301-4738.71673
Allmen R, Weiss S, Tevaearai H, Kuemmerli C, Tinner C, Carrel T, Schmidli J, Dick F (2015) Completeness of follow-up determines validity of study findings: results of a prospective repeated measures cohort study. PLoS One 10(10):e0140817. https://doi.org/10.1371/2Fjournal.pone.0140817
Ogunbayo O, Schafheutle E, Cutts C, Noyce P (2017) Self-care of long-term conditions: patients’ perspectives and their (limited) use of community pharmacies. Int J Clin Pharm 39(2):433–442. https://doi.org/10.1007/s11096-016-0418-y
Barker I, Steventon A, Williamson R, Deeny S (2018) Self-management capability in patients with long-term conditions is associated with reduced healthcare utilisation across a whole health economy: cross-sectional analysis of electronic health records. BMJ Qual Saf 27(12):989–999. https://doi.org/10.1136/bmjqs-2017-007635
Acknowledgements
The authors would like to acknowledge the assistance of Pauline Shaw, Health & Applied Sciences subject librarian at the University of the West of England, Bristol.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Palmer, S., Davey, I., Oliver, L. et al. The effectiveness of conservative interventions for the management of syndromic hypermobility: a systematic literature review. Clin Rheumatol 40, 1113–1129 (2021). https://doi.org/10.1007/s10067-020-05284-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05284-0