Abstract
The objective of the study was to examine the optimal Children’s Yale-Brown Obsessive–Compulsive Scale (CY-BOCS) percent reduction and raw cutoffs for predicting cognitive-behavioral treatment (CBT) response among children and adolescents with obsessive–compulsive disorder (OCD). The sample consisted of children and adolescents with OCD (N = 241) participating in the first step of the Nordic long-term OCD treatment study and receiving 14 weekly sessions of CBT in the form of exposure and response prevention. Evaluations were conducted pre- and post-treatment, included the CY-BOCS, Clinical Global Impressions—severity/improvement. The results showed that the most efficient CY-BOCS cutoffs were 35 % reduction for treatment response, 55 % reduction for remission, and a post-treatment CY-BOCS raw total score of 11 for treatment remission. Overall, our results diverge from previous research on pediatric OCD with more conservative cutoffs (higher cutoff reduction for response and remission, and lower raw score for remission). Further research on optimal cutoffs is needed.

Similar content being viewed by others
References
Rasmussen SA, Eisen JL (1992) The epidemiology and clinical features of obsessive compulsive disorder. Psychiatr Clin North Am 15:743–758
Ruscio AM, Stein DJ, Chiu WT, Kessler RC (2010) The epidemiology of obsessive–compulsive disorder in the national comorbidity survey replication. Mol Psychiatry 15:53–63
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, Faraone SV (2004) Long-term outcome of pediatric obsessive–compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiat Scand 110:4–13
Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D (1988) Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry 27:764–771
Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, Cuffe SP (1994) Frequency of obsessive–compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 33:782–791 (Erratum appears in J Am Acad Child Adolesc Psychiatry. 1995 Feb;34(2):128–129; PMID: 7896644)
Rapoport JL, Inoff-Germain G, Weissman MM, Greenwald S, Narrow WE, Jensen PS, Lahey BB, Canino G (2000) Childhood obsessive–compulsive disorder in the NIMH MECA study: parent versus child identification of cases. Methods for the epidemiology of child and adolescent mental disorders. J Anxiety Disord 14:535–548
Skarphedinsson G, Hanssen-Bauer K, Kornor H, Heiervang ER, Landro NI, Axelsdottir B, Biedilae S, Ivarsson T (2015) Standard individual cognitive behaviour therapy for paediatric obsessive–compulsive disorder: a systematic review of effect estimates across comparisons. Nord J Psychiatry 69:81–92
Ivarsson T, Skarphedinsson G, Kornor H, Axelsdottir B, Biedilae S, Heyman I, Asbahr F, Thomsen PH, Fineberg N, March J (2015) The place of and evidence for serotonin reuptake inhibitors (SRIs) for obsessive compulsive disorder (OCD) in children and adolescents: views based on a systematic review and meta-analysis. Psychiatry Res 227:93–103
Geller D, March J (2012) Practice parameter for the assessment and treatment of children and adolescents with obsessive–compulsive disorder. J Am Acad Child Adolesc Psychiatry 51:98–113
NICE (2005) Obsessive compulsive disorder (OCD) and body dysmorphic disorder (BDD). In: Excellence NIfHaC (ed) National Institute for Health and Clinical Excellence, London
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF (1997) Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852
Lewin A, Piacentini J (2010) Evidence-based assessment of child obsessive compulsive disorder: recommendations for clinical practice and treatment research. Child Youth Care Forum 39:73–89
Storch EA, Murphy TK, Bagner DM, Johns NB, Baumeister AL, Goodman WK, Geffken GR (2006) Reliability and validity of the child behavior checklist obsessive–compulsive scale. J Anxiety Disord 20:473–485
Lewin AB, Piacentini J, De Nadai AS, Jones AM, Peris TS, Geffken GR, Geller DA, Nadeau JM, Murphy TK, Storch EA (2014) Defining clinical severity in pediatric obsessive–compulsive disorder. Psychol Assess 26:679–684
Busner J, Targum SD (2007) The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry 4:28–37
Garvey MA, Perlmutter SJ, Allen AJ, Hamburger S, Lougee L, Leonard HL, Witowski ME, Dubbert B, Swedo SE (1999) A pilot study of penicillin prophylaxis for neuropsychiatric exacerbations triggered by streptococcal infections. Biol Psychiatry 45:1564–1571
Tolin DF, Abramowitz JS, Diefenbach GJ (2005) Defining response in clinical trials for obsessive–compulsive disorder: a signal detection analysis of the Yale-Brown obsessive compulsive scale. J Clin Psychiatry 66:1549–1557
Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM (1991) Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry 48:851–855
Pigott TA, Pato MT, Bernstein SE, Grover GN, Hill JL, Tolliver TJ, Murphy DL (1990) Controlled comparisons of clomipramine and fluoxetine in the treatment of obsessive–compulsive disorder. Behavioral and biological results. Arch Gen Psychiatry 47:926–932
Cottraux J, Note I, Yao SN, Lafont S, Note B, Mollard E, Bouvard M, Sauteraud A, Bourgeois M, Dartigues JF (2001) A randomized controlled trial of cognitive therapy versus intensive behavior therapy in obsessive compulsive disorder. Psychother Psychosom 70:288–297
Simpson HB, Gorfinkle KS, Liebowitz MR (1999) Cognitive-behavioral therapy as an adjunct to serotonin reuptake inhibitors in obsessive–compulsive disorder: an open trial. J Clin Psychiatry 60:584–590
Sookman D, Steketee G (2007) Directions in specialized cognitive behavior therapy for resistant obsessive–compulsive disorder: theory and practice of two approaches. Cognit Behav Pract 14:1–17
Wagner KD, Cook EH, Chung H, Messig M (2003) Remission status after long-term sertraline treatment of pediatric obsessive–compulsive disorder. J Child Adoles Psychopharmacol 13(Suppl 1):S53–S60
Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ, McCracken J (2011) Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive–compulsive disorder. J Am Acad Child Adolesc Psychiatry 50:1149–1161
POTS Study Team (2004) Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive–compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA 292:1969–1976
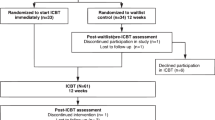
Torp NC, Dahl K, Skarphedinsson G, Thomsen P, Valderhaug R, Weidle B, Melin K, Hybel K, Nissen JB, Lenhard F, Wentzel-Larsen T, Franklin M, Ivarsson T (2015) Effectiveness of cognitive behavior treatment for pediatric obsessive–compulsive disorder: acute outcomes from the Nordic long-term OCD treatment study (NordLOTS). Behav Res Ther 64:15–23
Turner CM, Mataix-Cols D, Lovell K, Krebs G, Lang K, Byford S, Heyman I (2014) Telephone cognitive-behavioral therapy for adolescents with obsessive–compulsive disorder: a randomized controlled non-inferiority trial. J Am Acad Child Adolesc Psychiatry 53:1298–1307.e1292
Caporino NE, Brodman DM, Kendall PC, Albano AM, Sherrill J, Piacentini J, Sakolsky D, Birmaher B, Compton SN, Ginsburg G, Rynn M, McCracken J, Gosch E, Keeton C, March J, Walkup JT (2013) Defining treatment response and remission in child anxiety: signal detection analysis using the pediatric anxiety rating scale. J Am Acad Child Adolesc Psychiatry 52:57–67
Storch EA, Lewin AB, De Nadai AS, Murphy TK (2010) Defining treatment response and remission in obsessive–compulsive disorder: a signal detection analysis of the children’s Yale-Brown obsessive compulsive scale. J Am Acad Child Adolesc Psychiatry 49:708–717
Lewin AB, De Nadai AS, Park J, Goodman WK, Murphy TK, Storch EA (2011) Refining clinical judgment of treatment outcome in obsessive–compulsive disorder. Psychiatry Res 185:394–401
Swets JA, Pickett RM (1982) Evaluation of Diagnostic Systems: Methods from signal detection theory. Academic Press, New York
Thomsen PH, Torp NC, Dahl K, Christensen K, Englyst I, Melin KH, Nissen JB, Hybel KA, Valderhaug R, Weidle B, Skarphedinsson G, von Bahr PL, Ivarsson T (2013) The Nordic long-term OCD treatment study (NordLOTS): rationale, design, and methods. Child Adolesc Psychiatry Mental Health 7:41
Skarphedinsson G, Weidle B, Thomsen PH, Dahl K, Torp NC, Nissen JB, Melin KH, Hybel K, Valderhaug R, Wentzel-Larsen T, Compton SN, Ivarsson T (2015) Continued cognitive-behavior therapy versus sertraline for children and adolescents with obsessive–compulsive disorder that were non-responders to cognitive-behavior therapy: a randomized controlled trial. Eur Child Adolesc Psychiatry 24:591–602
American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition (Text Revision). American Psychiatric Association, Washington, DC
Torp NC, Dahl K, Skarphedinsson G, Thomsen PH, Valderhaug R, Weidle B, Hybel K, Compton S, Ivarsson T (2015) Predictors associated with improved cognitive-behavioral therapy outcome in pediatric obsessive–compulsive disorder. J Am Acad Child Adolesc Psychiatry 54:200–207
Kaufman J, Birmaher B, Brent D, Rao U et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
Lauth B, Arnkelsson GB, Magnusson P, Skarphedinsson G, Ferrari P, Petursson H (2010) Validity of K-SADS-PL (schedule for affective disorders and schizophrenia for school-age children-present and lifetime version) depression diagnoses in an adolescent clinical population. Nord J Psychiatry 64:409–420
Lauth B, Magnusson P, Ferrari P, Petursson H (2008) An Icelandic version of the kiddie-SADS-PL: translation, cross-cultural adaptation and inter-rater reliability. Nord J Psychiatry 62:379–385
Valderhaug R, Larsson B, Gotestam KG, Piacentini J (2007) An open clinical trial of cognitive-behaviour therapy in children and adolescents with obsessive–compulsive disorder administered in regular outpatient clinics. Behav Res Ther 45:577–589
Freeman JB, Garcia AM, Coyne L, Ale C, Przeworski A, Himle M, Compton S, Leonard HL (2008) Early childhood OCD: preliminary findings from a family-based cognitive-behavioral approach. J Am Acad Child Adolesc Psychiatry 47:593–602
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI (1997) Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852
Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P, Roberti JW, Killiany EM, Goodman WK (2004) Psychometric evaluation of the children’s Yale-Brown obsessive–compulsive scale. Psychiatry Res 129:91–98
Gallant J, Storch EA, Merlo LJ, Ricketts ED, Geffken GR, Goodman WK, Murphy TK (2008) Convergent and discriminant validity of the children’s Yale-Brown obsessive compulsive scale-symptom checklist. J Anxiety Disord 22:1369–1376
Guy W (1976) ECDEU assessment manual for psychopharmacology. Government Printing Office, Washington
Kraemer H, Periyakoil VS, Noda A (2002) Kappa coefficients in medical research. Stat Med 21:2109–2129
Kraemer H (1992) Evaluating medical tests: objective and quantitative guidelines. Sage Publications, Thousand Oaks
Pallanti S, Hollander E, Bienstock C, Koran L, Leckman J, Marazziti D, Pato M, Stein D, Zohar J, International Treatment Refractory OCDC (2002) Treatment non-response in OCD: methodological issues and operational definitions. Int J Neuropsychopharmacol 5:181–191
Leucht S, Davis JM, Engel RR, Kane JM, Wagenpfeil S (2007) Defining ‘response’ in antipsychotic drug trials: recommendations for the use of scale-derived cutoffs. Neuropsychopharmacology 32:1903–1910
Mataix-Cols D, de la Cruz LF, Nordsletten AE, Lenhard F, Isomura K, Simpson HB (2016) Towards an international expert consensus for defining treatment response, remission, recovery and relapse in obsessive–compulsive disorder. World Psychiatry 15:80–81
Farris SG, McLean CP, Van Meter PE, Simpson HB, Foa EB (2013) Treatment response, symptom remission, and wellness in obsessive–compulsive disorder. J Clin Psychiatry 74:685–690
Frank E, Kupfer DJ, Wagner EF, McEachran AB, Cornes C (1991) Efficacy of interpersonal psychotherapy as a maintenance treatment of recurrent depression: contributing factors. Arch Gen Psychiatry 48:1053–1059 [Erratum appears in Arch Gen Psychiatry 1992 May; 49(5):401]
Kennard BD, Emslie GJ, Mayes TL, Nakonezny PA, Jones JM, Foxwell AA, King J (2014) Sequential treatment with fluoxetine and relapse–prevention CBT to improve outcomes in pediatric depression. Am J Psychiatry 171:1083–1090
Franklin ME, Sapyta J, Freeman JB, Khanna M, Compton S, Almirall D, Moore P, Choate-Summers M, Garcia A, Edson AL, Foa EB, March JS (2011) Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive–compulsive disorder: the pediatric OCD treatment study II (POTS II) randomized controlled trial. J Am Med Assoc. 306:1224–1232
Eisen JL, Goodman WK, Keller MB, Warshaw MG, DeMarco LM, Luce DD, Rasmussen SA (1999) Patterns of remission and relapse in obsessive–compulsive disorder: a 2-year prospective study. J Clin Psychiatry 60:346–351 (quiz 352)
Leckman JF, Sholomskas D, Thompson D, Belanger A, Weissman MM (1982) Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 39:879–883
Højgaard DRMA, Mortensen E, Ivarsson T, Valderhaug R, Hybel K, Skarphedinsson G, Dahl K, Weidle B, Torp N, Grados M (2015) Child and adolescent OCD symptom patterns: a factor analytic study. In: 16th International ESCAP congress, Madrid, Spain, pp S187–S187
Acknowledgments
The authors would like to thank the patients and their parents that participated in the Nordic long-term OCD treatment study (NordLOTS) and the NordLOTS researcher group. Funding was applied to each national site as well as some central funding. We thank the following for their contributions: Trygfonden, The Danish Council for Strategic Research, Pulje til styrkelse af psykiatrisk forskning i Region Midtjylland, The Center for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP), Stiftelsen Clas Groschinskys Minnesfond, Norwegian Research Council, Norwegian ExtraFoundation, and (De Nadai) National Institutes of Health under Ruth L. Kirschstein National Research Service Award number F31MH094095 from the National Institute of Mental Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Tord Ivarsson is involved in Speakers Bureau for Shire, Sweden. Dr. Storch has received grant funding from NIH, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, the International OCD Foundation, and Ortho-McNeil Scientific Affairs Pharmaceuticals. He has received textbook honorarium from Springer, the American Psychological Association, Wiley Publishers, and Lawrence Erlbaum Associates. He is an educational consultant for Rogers Memorial Hospital. He serves as a consultant for Prophase, Inc. and CroNos, Inc., and serves on the Speaker’s Bureau and Scientific Advisory Board of the International OCD Foundation. He has received research support from the All Children’s Hospital Guild Endowed Chair. Dr. Adam Lewin Research support from the International OCD Foundation and All Children's Hospital. Honorarium from Oxford Press, Springer, and Children's Tumor Foundation. Travel Support from the Tourette Syndrome Association, American Psychological Association, Society for Clinical Child and Adolescent Psychology. Scientific Advisory Board for International OCD Foundation.
Rights and permissions
About this article
Cite this article
Skarphedinsson, G., De Nadai, A.S., Storch, E.A. et al. Defining cognitive-behavior therapy response and remission in pediatric OCD: a signal detection analysis of the Children’s Yale-Brown Obsessive Compulsive Scale. Eur Child Adolesc Psychiatry 26, 47–55 (2017). https://doi.org/10.1007/s00787-016-0863-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-016-0863-0