Abstract
Ethical and methodological factors limit the availability of data on metabolic and hormonal responses to exercise in children and adolescents. Despite this, it has been reported that young individuals show age-dependent responses to short and long term exercise when compared with adults.
Adenosine triphosphate (ATP) and phosphocreatine stores are not age-dependent in children and adolescents. However, phosphorus-31 nuclear magnetic resonance spectroscopy (31PNMR) studies showed smaller reductions in intramuscular pH in children and adolescents during high intensity exercise than adults. Muscle glycogen levels at rest are less important in children, but during adolescence these reach levels observed in adults.
Immaturity of anaerobic metabolism in children is a major consideration, and there are several possible reasons for this reduced glycolytic activity. There appear to be higher proportions of slow twitch (type I) fibres in the vastus lateralis part of the quadriceps in children than in untrained adults, and anaerobic glycolytic ATP rephosphorylation may be reduced in young individuals during high intensity exercise. Reduced activity of phosphofructokinase-1 and lactate dehydrogenase enzymes in prepubertal children could also explain the lower glycolytic capacity and the limited production of muscle lactate relative to adults. These observations may be related to reduced sympathetic responses to exhaustive resistance exercise in young people.
In contrast, children and adolescents are well adapted to prolonged exercise of moderate intensity. Growth and maturation induce increases in muscle mass, with proliferation of mitochondria and contractile proteins. However, substrate utilisation during exercise differs between children and adults, with metabolic and hormonal adaptations being suggested. Lower respiratory exchange ratio values are often observed in young individuals during prolonged moderate exercise. Data indicate that children rely more on fat oxidation than do adults, and increased free fatty acid mobilisation, glycerol release and growth hormone increases in preadolescent children support this hypothesis.
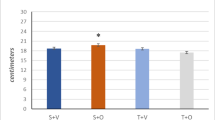
Plasma glucose responses during prolonged exercise are generally comparable in children and adults. When glucose is ingested at the beginning of moderate exercise, plasma glucose levels are higher in children than in adults, but this may be caused by decreased insulin sensitivity during the peripubertal period (as shown by glucose: insulin ratios).
Conclusions: Children are better adapted to aerobic exercise because their energy expenditure appears to rely more on oxidative metabolism than is the case in adults. Glycolytic activity is age-dependent, and the relative proportion of fat utilisation during prolonged exercise appears higher in children than in adults.
Similar content being viewed by others
References
Lac G, Duché P, Falgairette G, et al. Adrenal androgen profiles in saliva throughout puberty in both sexes. In: Coudert J, Van Praagh E, editors. Pediatric work physiology. XVI. Children and exercise. Paris: Masson, 1992: 221–3
Sizonenko PC, Paunier L. Hormonal changes in puberty III: correlation of plasma dehydroepiandrosterone, testosterone, FSH and LH with stages of puberty and bone age in normal boys and girls and in patients with Addison’s disease or hypogonadism or with premature or late adrenarche. J Clin Endocrinol Metab 1975; 41 (5): 894–904
Martha PM, Gorman KM, Blizzard RM, et al. Endogenous growth hormone secretion and clearance rates in normal boys, as determined by deconvolution analysis: relationship to age pubertal status and body mass. J Clin Endocrinol Metab 1992; 74: 336–44
Bar-Or O. Pediatric sports medicine for the practitioner. New York: Springer Verlag, 1983
Rowland TW. Developmental aspects of physiological function relating to aerobic exercise in children. Sports Med 1990; 10 (4): 255–66
Armstrong N, Welsman JR. Developmental aspects of aerobic fitness in children and adolescents. In: Holloszy JO, editor. Exercise and sport sciences reviews. Baltimore (MD): Williams & Wilkins, 1994: 435–76
Keizer H, Poortman J, Bunnik GS. Influence of physical exercise on sex-hormone metabolism. J Appl Physiol 1980; 48 (5): 765–9
Wilkerson JE, Horvath SM, Gutin B. Plasma testosterone during treadmill running. J Appl Physiol 1980; 49 (2): 249-53
Lemon PWR, Nagle FJ. Effect of exercise on protein and amino acid metabolism. Med Sci Sports Exerc 1981; 13: 141–9
Wilmore JH, Costill DL. Physiology of sport and exercise. 2nd ed. Champaign (IL): Human Kinetics, 1999
Sapega AA, Sokolow DP, Graham TJ, et al. Phosphorus nuclear magnetic resonance: a non-invasive technique for the study of muscle bioenergetics during exercise. Med Sci Sports Exerc 1987; 19 (4): 410–20
Zanconato S, Buchthal S, Barstow TJ, et al. 31P-magnetic resonance spectroscopy of leg muscle metabolism during exercise in children and adults. J Appl Physiol 1993 May; 74 (5): 2214–8
Kuno S, Miyamaru M, Itai J. Muscle energetics during exercise of elite sprinter in children by 31PNMR. Med Sci Sports Exerc 1993; 25 Suppl. 5: S175
Kuno S, Takahashi H, Fujimoto K, et al. Muscle metabolism during exercise using phosphorus-31 nuclear magnetic resonance spectroscopy in adolescents. Eur J Appl Physiol Occup Physiol 1995; 70 (4): 301–4
Petersen SR, Gaul CA, Stanton NM, et al. Skeletal muscle metabolism during short-term, high-intensity exercise in prepubertal and pubertal girls. J Appl Physiol 1999; 87 (6): 2151–6
Cooper DM. Development of the oxygen transport system in normal children. In: Bar-Or O, editor. Advances in pediatric sport sciences: biological issues. 3. Champaign (IL): Human Kinetics, 1989: 67–100
Williams CA. Children’s and adolescents’ anaerobic performance during cycle ergometry. Sports Med 1997; 24: 227–40
Falize J. Le développement moteur de l’enfant: perspectives d’application. In: De Potter JC, Levarlet H, editors. Développement moteur et éducation. Brussels: Presses Universitaires de Bruxelles, 1984: 47–66
Falgairette G, Bedu M, Fellmann N, et al. Bioenergetic profile in 144 boys age from 6 to 15 years with special reference to sexual maturation. Eur J Appl Physiol Occup Physiol 1991; 62 (3): 151–6
Duché P, Falgairette G, Bedu M, et al. Longitudinal approach of bioenergetic profile in boys before and during puberty. In: Coudert J, Van Praagh E, editors. Pediatric work physiology. XVI. Children and exercise. Paris: Masson, 1992: 43–5
Mercier B, Mercier J, Granier P, et al. Maximal anaerobic power: relationship to anthropometric characteristics during growth. Int J Sports Med 1992; 13: 21–6
Allen RE, Merkel RA, Young RB. Cellular aspects of muscle growth: myogenic cell proliferation. J Anim Sci 1979; 49 (1): 115–27
Colling-Saltin AS. Enzyme histochemistry on skeletal muscle of the human foetus. J Neurol Sci 1978; 39: 169–85
Elder GCB, Kakukas BA. Histochemical and contractile property changes during human muscle development. Muscle Nerve 1993; 16 (11): 1246–53
Vogler C, Bove KE. Morphology of skeletal muscle in children. Arch Pathol Lab Med 1985; 109: 238–42
Bell RD, MacDougall JD, Billeter R, et al. Muscle fibres types and morphometric analysis of skeletal muscle in six years old children. Med Sci Sports Exerc 1980; 12 (1): 28–31
Fournier M, Ricci J, Taylor AW, et al. Skeletal muscle adaptation in adolescent boys: sprint and endurance training and detraining. Med Sci Sports Exerc 1982; 14 (6): 453–6
Mero A, Jaakkola L, Komi PV. Relationships between muscle characteristics and physical performance capacity in trained athletic boys. J Sports Sci 1991; 9: 161–71
Eriksson O, Saltin B. Muscle metabolism during exercise in boys aged 11 to 16 years compared to adults. Acta Paediatr Belg 1974; 28 Suppl.: 257–65
Gollnick PD, Armstrong RB, Saubert CW, et al. Enzyme activity and fiber composition in skeletal muscle of untrained and trained men. J Appl Physiol 1972; 33 (3): 312–9
Hedberg G, Jansson E. Skeletal muscle fibre distribution, capacity and interest in different physical activities among students in high school [Swedish]. Pedagogiska Rapporter 1976: 54
du Plessis M, Smit P, du Plessis L, et al. The composition of muscle fibers in a group of adolescents. In: Binkhorst RA, Kemper HCG, Saris WHH, editors. Children and exercise. XI. Champaign (IL): Human Kinetics, 1985: 323–8
Houmard JA, Smith R, Jendrasiak GL. Relationship between MRI relaxation time and muscle fibre composition. J Appl Physiol 1995; 78: 807–9
Parkkola R, Alanen A, Klimo H, et al. MR relaxation times and fiber type predominance of the psoas and multifidus muscle. Acta Radiol 1993; 34: 16–9
Kuno S, Katsuta S, Inouye T, et al. Relationship between MR relaxation time and muscle fiber composition. Radiology 1988; 169: 657–68
Colling-Saltin AS. Some quantitative biochemical evaluation of developing skeletal muscle in the human foetus. J Neurol Sci 1978; 39: 187–98
Eriksson BO, Karlsson J, Saltin B. Muscle metabolites during exercise in pubertal boys. Acta Paediatr Scand 1971; 217 Suppl.: 154–7
Bougnères PF. Rôle des substrats lipidiques dans l’adaptation au jeune du nouveau-né et de l’enfant. J Annu Diabetol Hotel Dieu 1988: 303–14
Schiffrin A, Colle E. Hypoglycemia. In: Collin R, Ducharme JR, editors. Pediatric endocrinology. New-York: Raven Press, 1989: 649–73
Eriksson BO, Gollnick PD, Saltin B. Muscle metabolism and enzyme activities after training in boys 11–13 years old. Acta Physiol Scand 1973; 87: 485–97
Haralambie G. Enzyme activities in skeletal muscle of 13–15 years old adolescents. Bull Eur Physiopathol Respir 1982; 18 (1): 65–74
Mero A. Measurement of aerobic and anaerobic performance capacity in young boys. In: Coudert J, Van Praagh E, editors. Pediatric work physiology. XVI. Children and exercise. Paris: Masson, 1992: 19–21
Eriksson BO. Physical training, oxygen supply and muscle metabolism in 11–13 year old boys. Acta Physiol Scand 1972; 384 Suppl.: 1–48
Berg A, Kim SS, Keul J. Skeletal muscle enzyme activities in healthy young subjects. Int J Sports Med 1986; 4: 236–9
Falgairette G, Bedu M, Fellmann N, et al. Modifications of aerobic and anaerobic metabolism in active boys during puberty. In: Beunen G, Ghesquiere J, Reybrouk T, et al., editors. Children and exercise. IV. Stuttgart: Ferdinand Enke Verlag, 1990: 42–9
Rostein A, Dofan R, Bar-Or O, et al. Effect of training on anaerobic threshold, maximal aerobic power and anaerobic performance of preadolescent boys. Int J Sports Med 1986; 7 (5): 281–6
Rilling JK, Worthman CM, Campell BC, et al. Ratios of plasma and salivary testosterone throughout puberty: production versus bioavailability. Steroids 1996; 61 (6): 374–8
Crielaard JM, Pirnay F, Franchimont P. Croissance et exercice anaérobie lactique. In: Benezis C, Simeray J, Simon L, editors. L’enfant, l’adolescent et le sport, actualités en médecine du sport. Paris: Masson, 1986: 33–51
Von Diter H, Nowacki P, Simai E, et al. Das Verhalten des Säure-Basen-Haushalts nach erschöpfender Belastung bei untrainierten und tranierten Jungen und Mädchenim Vergleich zu Leistungssportlern. Sportarzt Sportmed 1977; 28: 45–8
Matejkova J, Kroprikova Z, Placheta Z. Changes in acid-base balance after maximal exercise. In: Placheta Z, editor. Youth and physical activity. Purkyne (Czechoslovakia): JE University, 1980: 191–9
Galbo H. Autonomic neuroendocrine responses to exercise. Scand J Sports Sci 1986; 8 (1): 3–17
Richter EA, Ruderman NB, Galbo H. Alpha and beta adrenergic effects on metabolism in contracting perfused muscle. Acta Physiol Scand 1982; 116: 215–22
Spriet L, Ren JM, Hultman E. Epinephrine infusion enhances muscle glycogenolysis during prolonged electrical stimulation. J Appl Physiol 1988; 64: 1439–44
Kindermann W, Schnabel A, Schmitt WM, et al. Catecholamines, growth hormone, cortisol, insulin and sex hormone in anaerobic and aerobic exercise. Eur J Appl Physiol 1982; 49: 389–99
Lehmann M, Keul J, Da Prada M, et al. Plasmakatecholamine, glucose, lactat und sauerstoffaufnahmefähikeit von kindern bei aeroben und anaeroben bealastungen. Dtsch Z fur Sportmed 1980; 8: 230–6
Pullinen T, Mero A, Mac Donald E, et al. Plasma catecholamine and serum testosterone responses to four units of resistance exercise in young and adult male athletes. Eur J Appl Physiol 1998; 77: 413–20
Boobis LH, Williams C, Wooton SA. Influence of sprint training on muscle metabolism during brief maximal exercise in man [abstract]. J Physiol (Lond) 1983; 342: 36–7
Nevill ME, Boobis LH, Brooks S, et al. Effect of training on muscle metabolism during treadmill sprinting. J Appl Physiol 1989; 67: 2376–82
Eriksson BO. Muscle metabolism in children: a review. Acta Paediatr Scand 1980; 283 Suppl.: 20–8
Thorstensson A, Sjodin B, Karlsson J. Enzyme activities and muscle strength after sprint training in man. Acta Physiol Scand 1975; 94: 313–8
Hebestreit H, Mimura k, Bar-Or O. Recovery of anaerobic muscle power following 30s supramaximal exercise: comparison between boys and men. J Appl Physiol 1993; 74: 2875–80
Hebestreit H, Meyer F, Htay-Htay G, et al. Plasma electrolyte and hydrogen ion levels following a 30s high intensity task: boys vs men [abstract no. 1183]. Med Sci Sports Exerc 1994; 26 Suppl.: S210
Astrand PO, Rodhal K. Textbook of work physiology. New York: McGraw-Hill, 1986
Martinez LR, Haymes EM. Substrate utilization during treadmill running in prepubertal girls and women. Med Sci Sports Exerc 1992; 24 (9): 975–83
Asano K, Hirakoba K. Respiratory and circulatory adaptation during prolonged exercise in 10- to 12-year-old children and in adults. In: Imaarinen J, Vaalimaki I, editors. Children and sport. Berlin: Springer-Verlag, 1984: 119–28
Eynde BV, Van Gerven D, Vienne D, et al. Endurance fitness and peak height velocity in Belgian boys. In: Oseid S, Caarlsen K, editors. Children and exercise. XIII. Champaign (IL): Human Kinetics, 1989: 19–27
Robinson S. Experimental studies of physical fitness in relation to age. Int Z Angew Physiol Einschl Arbeitphysiol 1938; 10: 251–323
Morse M, Schltz FW, Cassels E. Relation of age to physiological responses of the older boys (10–17 years) to exercise. J Appl Physiol 1949; 1: 638–709
Montoye H. Age and oxygen utilization during submaximal treadmill exercise in males. J Gerontol 1982; 37: 396–402
Rowland TW, Auchinachie JA, Keenan TJ, et al. Physiological responses to treadmill running in adult and prepubertal males. Int J Sports Med 1987; 8: 292–7
Rowland TW, Rimany TA. Physiological responses to prolonged exercise in premenarcheal and adult females. Pediatr Exerc Sci 1995; 7: 183–91
Macek M, Vavra J, Novosadova J. Prolonged exercise in prepubertal boys II. Changes in plasma volume and in some blood constituents. Eur J Appl Physiol 1976; 35: 299–303
Van Beaumont W. Evaluation of hemoconcentration from hematocrit measurements. J Appl Physiol 1972; 32: 712–3
Hill DB, Costill DL. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 1974; 37: 299–303
Fahey TD, Del Valle-Zuris, Oehlsen G, et al. Pubertal stage differences in hormonal and hematological responses to maximal exercise in males. J Appl Physiol 1979; 46 (4): 823–7
Astrand PO, Saltin B. Plasma and red cell volume after prolonged severe exercise. J Appl Physiol 1964; 19: 829–32
Flandrois R. Conséquences de l’exercice de longue durée sur l’hydratation de l’organisme: réactions hormonales. In: Lacour JR, editor. Comptes-rendus du colloque de Saint-Etienne. Facteurs limitant l’endurance humaine. Paris: Masson, 1977: 38–42
Melin B, Eclache JP, Geelen G, et al. Plasma AVP, neurophysin, renin activity and aldosterone during submaximal exercise performed until exhaustion in trained and untrained men. Eur J Appl 1980; 44: 141–51
Delamarche P, Monnier M, Gratas-Delamarche A, et al. Glucose and free fatty acid utilization during prolonged exercise in prepubertal boys in relation to catecholamine responses. Eur J Appl Physiol 1992; 65: 66–72
Davies CTM. Thermal responses to exercise in children. Ergonomics 1981; 48: 55–61
Delamarche P, Bittel J, Lacour JR, et al. Thermoregulation at rest and during exercise in prepubertal boys. Eur J Appl Physiol 1990; 60: 436–40
Sjodin B, Schele R, Karlsson J, et al. The physiological background of onset blood lactate accumulation. International series on sports sciences. Vol. 12. Exercise and sport biology. Champaign (IL): Human Kinetics, 1982
Sjodin B, Jacobs I. Onset of blood lactate accumulation and marathon running performance. Int J Sport Med 1981; 2: 23–6
Sjodin B, Jacobs I, Svedenhag J. Changes in onset blood lactate accumulation and muscle enzymes after training at OBLA. Eur J Appl Physiol 1982; 49: 45–57
Mocellin R, Heusgen M, Korsten-Reck U. Maximal steady state blood lactate levels in 11-year-old boys. Eur J Pediatr 1990; 149: 771–3
Mocellin R, Heusgen M, Gildein HP. Anaerobic threshold and maximal steady-state blood lactate in prepubertal boys. Eur J Appl Physiol 1991; 62: 56–60
Williams JR, Armstrong N, Kirby BJ. The 4mM blood lactate level as an index of exercise performance in 11–13 year old children. J Sports Sci 1990; 8: 139–47
Tolfrey K, Armstrong N. Child-adult differences in whole blood lactate responses to incremental treadmill exercise. Br J Sports Med 1995; 29 (3): 196–9
Farrel PA, Wilmore JH, Coyle EF, et al. Plasma lactate accumulation and distance running performance. Med Sci Sports Exerc 1979; 11: 338–44
Amiel S, Sherwin R, Simonson D, et al. Impaired insulin action in puberty a contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med 1986; 315: 215–9
Bloch C, Clemons P, Sperling M. Puberty decreases insulin sensitivity. J Pediatr 1987; 110: 481–7
Cook J, Hoffman R, Stene M,et al. Effects ofmaturational stage on insulin sensitivity during puberty. J Clin Endocrinol Metab 1993; 77: 725–30
Oseid S, Hermansen L. Hormonal and metabolic changes during and after prolonged muscular work in prepubertal boys. Acta Paediatr Scand 1971; 217 Suppl.: 147–53
Eriksson BO, Persson B, Thorell JI. The effects of repeated prolonged exercise on plasma growth hormone, insulin, glucose, free fatty acids, glycerol, lactate and β-hydroxybutyric acid in 13-year old boys and in adults. Acta Paediatr Scand 1971; 217 Suppl.: 142–6
Wirth A, Trager E, Scheele K, et al. Cardiopulmonary adjustment and metabolic response to maximal and submaximal physical exercise of boys and girls at different stages of maturity. Eur J Appl Physiol 1978; 39: 229–40
Delamarche P, Gratas-Delamarche A, Monnier M, et al. Glucoregulation and hormonal changes during prolonged exercise in boys and girls. Eur J Appl Physiol 1994; 68: 3–8
Hoelzer DR, Dalsky GP, Clutter WE, et al. Glucoregulation during exercise: hypoglycaemia is prevented by redundant glucoregulatory systems, sympathochromaffin activation and changes in islet hormone secretion. J Clin Invest 1986; 77: 212–21
Boisseau N, Rannou F, Delamarche P, et al. Peripubertal period decreases insulin sensitivity and glucose utilisation during exercise. In: N Armstrong, J Welsman, editors. Children and exercise. XIX. London: E & FN Spon, 1997: 413–7
Boisseau N, Rannou F, Gratas-Delamarche A, et al. La tolerance au glucose à l’exercice prolongé chez la petite fille prépubère. Sci Sports 1999; 14: 173–9
Arslanian SA, Kalhan SC. Correlations between fatty acid and glucose metabolism. Potential explanation of insulin resistance of puberty. Diabetes 1994; 43: 908–14
Lehmann M, Keul J, Hesse A. Zur aeroben und anaeroben kapazität sowie catecholamine exkretion von kindern und jugendlichen während langdauernder submaximaler Körperarbeit. Eur J Appl Physiol 1982; 8: 135–45
Costill DL, Fink WJ, Getchell LH, et al. Lipid metabolism in skeletal muscle of endurance-trained males and females. J Appl Physiol 1979; 61: 1796–801
Berg A, Keul J, Huber G. Biochemische akutveranderunggen bei ausdauerbelastungen im kindes- und jugendalter. Monatsschr Kinderheilkd 1980; 128: 490–5
Haralambie G. Skeletal muscle enzymee activities in female subjects of various ages. Bull Eur Physiopathol Respir 1979; 15: 259–67
Nesher R, Karl IE, Kipnis DM. Dissociation of effects of insulin and contraction on glucose transport in rat epitrochlearis muscle. Am J Physiol 1985; 249 (3 Pt 1): C226–32
Holloszy JO, Hansen PA. Regulation of glucose transport into skeletal muscle. Rev Physiol Biochem Pharmacol 1996; 128: 99–193
Goodyear LJ, Kahn BB. Exercise, glucose transport, and insulin sensitivity. Annu Rev Med 1998; 49: 235–61
Wallberg-Henriksson H. Exercise and diabetes mellitus. Exerc Sports Sci Rev 1992; 20: 339–68
Richter EA, Galbo H, Sonne B, et al. Adrenal medullary control of muscular and hepatic glycogenolysis and of pancreatic hormonal secretion in exercising rats. Acta Physiol Scand 1980; 108: 235–42
Caprio S, Plewe G, Diamond M, et al. Increased insulin secretion in puberty: a compensatory response to reductions in insulin sensitivity. J Pediatr 1989; 114: 963–7
Galbo H. Endocrine factors in endurance. In: Shepard RJ, Astrand PO, editors. Endurance in sport. Oxford: Blackwell scientific publications, 1992
Lehmann M, Keul J, Korsten-Reck V. Einfluß einer stufenweisen laufbanderergometrie bei kinder und erwachsenen auf die plasmacatecholamine, die aerobe und anaerobe kapazitat. Eur J Appl Physiol Occup Physiol 1981; 47 (3): 301–11
Fleg JL, Tzankoff SP, Lakatta EG. Age related augmentation of plasma catecholamines during dynamic exercise in healthy males. J Appl Physiol 1985; 59: 1033–9
Lehmann M, Keul J. Age-associated changes of exercise-induced plasma catecholamines responses. Eur J Appl Physiol Occup Physiol 1986; 55 (3): 302–6
Rowland TW, Maresh CM, Charkoudian N, et al. Plasma norepinephrine responses to cycle exercise in boys and men. Int J Sports Med 1996; 17 (1): 22–6
Marin G, Domené HM, Barnes KM, et al. The effects of estrogen priming and puberty on the growth hormone response to standardized treadmill exercise and arginine-insulin in normal girls and boys. J Clin Endocrinol Metab 1994; 79 (2): 537–41
Bouix O, Brun JF, Fedou C, et al. Plasma beta-endorphin, corticotrophin and growth hormone to exercise in pubertal and prepubertal children. Horm Metab Res 1994; 26 (4): 195–9
Treolar AE, Boynton RE, Behn BG, et al. Variation of human menstrual cycle through reproductive life. Int J Fertil 1967; 12: 77–126
Viru A, Laaneots L, Karelson K, et al. Exercise-induced hormone responses in girls at different stages of sexual maturation. Eur J Appl Physiol Occup Physiol 1998; 77 (5): 401–8
Viru A, Viru M, Kuusler K, et al. Exercise-induced hormonal responses in boys in relation to sexual maturation [poster-abstract]. In: XXth international symposium of the European group of Pediatric Work Physiology; 1999 Sep 15–19; Sabaudia, 135
Cacciari E, Mazzanti L, Tassinari D, et al. Effects of sport (football) on growth: auxological, anthropometric and hormonal aspects. Eur J Appl Physiol Occup Physiol 1990; 61 (1–2): 149–58
Mero A, Jaakkola L, Komi PV. Serum hormones and physical performance capacity in young boys athletes during a 1-year training period. Eur J Appl Physiol Occup Physiol 1990; 60 (1): 32–7
Rowland TW, Morris AH, Kelleher JF, et al. Serum testosterone response to training in adolescent runners. Am J Dis Child 1987; 141: 881–3
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Boisseau, N., Delamarche, P. Metabolic and Hormonal Responses to Exercise in Children and Adolescents. Sports Med 30, 405–422 (2000). https://doi.org/10.2165/00007256-200030060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00007256-200030060-00003